The NHS is taking ‘radical’ measures as it steps up the fight against cancer – but it could lead to the GP gatekeeper role being completely sidelined.
Managers are planning to test whether allowing patients to bypass GPs and refer themselves for tests will speed up diagnosis times, with a view to rolling this out nationwide.
But Pulse has learned that a recent pilot in Leeds found most lung cancers were diagnosed following referral for chest X-rays by GPs, rather than through self-referral by patients.
The plan comes at a time when NHS England says survival rates are at their highest and official figures show GP referrals for suspected cancer are increasing.
And NICE has already launched a consultation on lowering the recommended threshold for cancer referrals.
Experts have warned this latest initiative has the potential to harm patients by increasing unnecessary investigations.
But NHS England believes the proposal – alongside seven other new initiatives – will help save thousands of lives a year in England.
Five-year strategy
Managers announced last month the launch of a new five-year cancer strategy in the summer, led by a taskforce that includes representatives from the RCGP and Cancer Research UK.
But in the meantime they intend to test several new approaches to speed up cancer diagnosis, with the aim of rolling them out nationally in 2016/17.
NHS England says it wants to deliver a 10% increase in the proportion of patients diagnosed at an early stage – from 50% of cases to 60% – an improvement it estimates will mean 8,000 more patients survive at least five years after diagnosis.
To achieve this, a number of initiatives are to be tested at some 60 different sites across the country. These include offering GPs greater direct access to rapid diagnostics, the introduction of bespoke clinics to send patients for several exploratory tests in a single visit and creating a pathway for patients with vague symptoms, such as tiredness or unexplained weight loss. There will also be £15m of new investment in new radiotherapy technology.
NHS England chief executive Simon Stevens says: ‘Cancer survival rates are at an all-time high, but too many patients are still being diagnosed late – up to one in four only when they present in A&E.’ It’s time for a ‘fresh look’, he says, ‘so we can save at least 8,000 lives a year’.
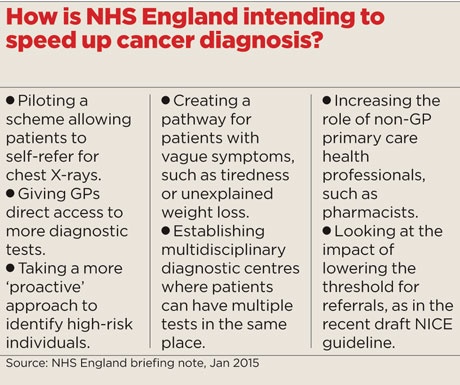
One such ‘fresh look’ is to consider allowing patients to self-refer. NHS England has not yet provided details but it has told Pulse that the scheme is being piloted in one area – Mid Cheshire.
It will involve offering people from areas of Crewe that have high incidences of lung cancer, and where uptake of health services has traditionally been poor, the opportunity to request a chest X-ray for themselves.
NHS England says: ‘Enabling patients to book their own appointments directly with a diagnostic testing unit or hospital diagnostic service could remove the need for them to see their GP, potentially speeding up the process of diagnosis.’
Although this is the first scheme of its type to be piloted by NHS England, a similar chest X-ray self-referral approach has already been trialled in Leeds, where it is now part of routinely commissioned cancer services.
Since 2010, people aged over 50 who have had a cough for three weeks or longer have been able to present at hospital to request a chest X-ray without first getting referred by their GP, as part of a package of measures to improve early detection.
Dr Adrian Rees, clinical lead for cancer at NHS Leeds West CCG, says the approach is still under evaluation but already seems to have had an impact on cancer outcomes.
He says: ‘Provisional data show an improvement in one-year survival from lung cancer, a reduction in hospital bed days, a fall in emergency presentations of lung cancer and a small improvement in presenting stage of disease.’

‘The GP role as a gatekeeper has been undermined’
Dr Kailash Chand, deputy chair of the BMA
But Dr Richard Vautrey, GPC deputy chair and a GP in Leeds, says: ‘While a small number of lung cancers were detected, I don’t think they were at a significantly earlier stage than would have been the case from direct GP referrals, and so the long-term outcome for patients was not that different despite the additional expense.’
Pulse also spoke with Dr Matthew Callister, consultant respiratory physician at Leeds Teaching Hospitals NHS Trust and lead researcher on the programme.
He says: ‘I think self-referral has been a useful aspect of the programme. We have shown that patients are able to use the service appropriately, and our local GPs have been very supportive of the new pathway.
‘Patients are recalled directly for CT in case of an abnormal X-ray, and patient feedback has been excellent.
‘However, even with the self-referral pathway, most patients were diagnosed with lung cancer following referral from their GP. Our experience would therefore support introducing a self-referral pathway, but only as part of a wider campaign incorporating GP training, lowering referral thresholds and community education.’
And some GPs are highly sceptical about the approach in principle. Dr Kailash Chand, deputy chair of the BMA and a retired GP in Lancashire, warns it risks eroding GPs’ vital role as ‘gatekeepers’ to diagnostic tests.
Dr Chand says: ‘For the past 10 to 15 years, the GP role as a gatekeeper has been undermined by the likes of walk-in centres. This is now going full steam. I won’t be surprised if politicians start saying we don’t need GPs.’
There are also concerns that allowing people to refer themselves for chest X-rays or other diagnostic tests will inevitably increase the number of unnecessary investigations people undergo.
Dr Andrew Green, chair of the GPC’s clinical prescribing subcommittee believes self-referral is unlikely to help, while the potential for harm is ‘significant’.
He says: ‘Self-referral is contentious, and my personal belief is it is unlikely to help. Any delay of a few days caused by the need for GP involvement will not turn a patient from treatable to untreatable, and the harms caused by over-investigation are likely to be significant.’
Others warn GPs could be left to deal with the ‘fall-out’ from patients seeking further follow-up appointments.
Dr Andrew Mimnagh, GP and urgent care lead at NHS Sefton CCG, says: ‘The direct service must manage the repeated attendances for rechecking and not deflect them on to the GP.’
Referrals bounced
The move will also add to concerns about demand on the health service, with diagnostic services already under strain.
Pulse recently reported that GPs are having urgent cancer referrals bounced or downgraded, as CCGs and acute trusts attempt to manage soaring demand.
A new report from the National Audit Office, published in January, highlighted this pattern once more.
Survival rates have been steadily improving, it found, with 69% of people diagnosed in 2012 surviving 12 months compared with 65% in 2007. It also found a 51% increase in urgent GP referrals over the past five years – seen as a major factor in the improvement.
But the report also shows services are now struggling to cope: nationally, the Government’s 62-day treatment target has not been met for more than a year, while survival rates remain around 10% lower than the European average.
The report says: ‘The waiting time standard that 85% of patients should be treated within 62 days of an urgent GP referral has not been achieved since September to December 2013.’
Meanwhile, new NICE draft guidelines on cancer referrals propose reducing the risk threshold, which GP experts say will increase demand on struggling services.
As such, the profession will want to see evidence that the self-referral scheme will be adequately funded to prevent these delays getting worse and other services suffering.
Dr Maureen Baker, chair of the RCGP and a member of the new cancer taskforce, cites this potential knock-on effect as a key concern.
She says: ‘We are prepared to look at all the proposals, but in the case of self-referral we would need to understand how it could work effectively without diverting resources from other services.’
Leeds cancer scheme – ‘Most of the increase came from GP referrals’
Leeds has had a worse cancer survival than the UK average, which in turn has historically lagged behind international averages.
To try to tackle this inequality, in 2010 NHS Leeds and Leeds Teaching Hospitals NHS Trust set up a pilot to improve early detection of lung cancer under the auspices of the National Awareness and Early Diagnosis Initiative and with funding from the Department of Health.
This involved a ‘Got a cough?, Get a Check’ campaign to raise awareness of lung cancer symptoms, with advertising and community education programmes targeting deprived areas.
GP education sessions
The programme included GP education sessions aimed at lowering the threshold for suspicion of lung cancer and increasing chest X-ray referrals.
Alongside this, a self-referral chest X-ray service was set up, whereby people over 50 who have had a cough for three weeks or longer can self-present at the hospital, without a GP referral to request a chest X-ray. Those with an abnormal chest X-ray were automatically recalled for a CT scan with automatic onward referral to the lung cancer multidisciplinary meeting.
There was a big increase in chest X-rays, from around 20,000 to 30,000 a year. Most of the increase came from a rise in GP referrals, with around 2,500 coming via self-referral. Most patients were diagnosed following GP referral.
Provisional data show an improvement in one-year survival, a reduction in hospital bed days, a decrease in emergency presentations of lung cancer and a small improvement in presenting stage of disease.
The project has now been running for five years and is commissioned as part of routine practice in Leeds. The CCG is in the process of redesigning wider cancer services for Leeds.
Dr Matthew Callister, consultant respiratory physician at Leeds Teaching Hospitals NHS Trust and leader of the cancer diagnosis scheme.