Some are describing it as a new era of ‘statinisation’.
Last month NICE fired the starting gun on a race to place millions more patients on statins by halving the threshold for primary prevention to a 10%10-year risk of heart disease.
The US is already working to a 7.5% primary prevention threshold and with the cost of generic atorvastatin plummeting, the Joint British Societies are due to recommend within weeks that GPs place even younger patients on statins if they have a high ‘lifetime risk’ of a cardiovascular (CV) event.
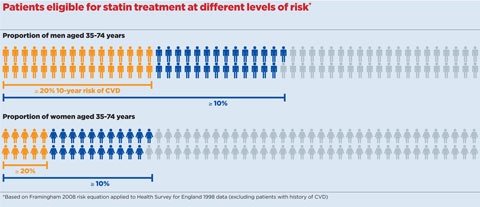
According to experts’ estimates, the proposal from NICE in its draft guideline on lipid modification to lower the CV risk threshold from 20% to 10% will mean a statin should be offered to more than 80% of men over 50 and half of women over 60.1
This would signal an unprecedented drive to prescribe statins in people yet to experience a CV event. Estimates suggest the number of patients on the drugs will rise from five million to 12 million.2
But GPs remain unconvinced by the evidence and are worried about the additional workload. A Pulse survey of 511 GPs reveals 57% of the profession do not support the draft guidance, while only 25% do support it. Even more strikingly, more than half (55%) would not take a statin themselves – or recommend a family member to do so – if they had a 10% 10-year CV risk. Just 29% would. However, 50% said they would adhere to the 10% threshhold if it is included in NICE’s final guideline; only 15% said they would not.
The evidence
NICE argues treatment with the high-intensity statin atorvastatin at a daily dose of 20mg ‘is clinically and cost effective’ for the primary prevention of cardiovascular disease (CVD) for those with a 10% or greater risk over 10 years, although it refuses to release its own full impact assessment of the change before the final guidance is published in July.
But even enthusiasts are nervous about the draft guidance, suggesting NICE may be going too far down the pharmacological route, and warning many patients will be placed on a statin due to the risk conferred by age alone.
The latest evidence does indicate that statins reduce the risk of heart attacks and strokes even at very low risk.
One large meta-analysis from Oxford University researchers, published in The Lancet in 2012, showed statin treatment reduced CV events and death over five years among people even at lower risks – below the 10% 10-year risk cut-off – and that the benefits exceeded any known hazards of statin therapy.3
On the back of a growing body of published evidence, US guidelines from the American College of Cardiology and American Heart Association – which adopted a 10% risk threshold a decade ago – went even further at the end of 2013 and recommended statins for people with a 7.5% 10-year CV risk, potentially putting one in three US adults on a statin.
But others argue the benefits of statins do not outweigh the risks at lower risk thresholds. A recent BMJ paper showed statin therapy only prevented one serious CV event for every 140 low-risk (<10%) people treated for five years, contrasting this with an 18% risk of side-effects.4
Age-related risk
Dr Kathryn Griffith, a GPSI in cardiology in York, says she is worried the NICE guidance will automatically class too many older people as being high-risk.
She says: ‘I am concerned that perhaps things have gone too far. All my older patients are at increased CV risk because of age rather than, for example, cholesterol levels, and they will all be over 10% risk. In their 90s they have passed the risk of premature heart disease and moved beyond the evidence from any clinical trial.
‘I think we should avoid offering a treatment to a group of the population whose only risk is related to their age and for whom there is no outcome evidence. This group of patients are also those who are most likely to suffer side-effects.’
But experts claim this misses the point. Professor Colin Baigent, professor of epidemiology and honorary consultant in public health at the University of Oxford, says: ‘It is true your risk will get above a certain level at a certain age, so these guidelines will tend to include older people – but they will tend to be at higher risk.
‘Younger people will only be offered treatment if they have multiple factors, for example, if they have a family history, smoke, are overweight or have high blood pressure – they’d have to have several of those things. So in general, the risk equations GPs are being asked to use will identify people most at risk.’
Practice workload is also a major concern. NICE recommends a ‘systematic approach’ to identify people at high risk in the age range 40 to 74 years, and that all those aged 85 years or over should be considered for statin treatment.
Of the GPs who responded to Pulse’s survey, 79% said that the shift to a 10% threshold would represent a ‘major’ or ‘significant’ increase in workload. More than a third (34%) would have to switch from Framingham to QRISK2 to calculate CV risk to conform with the draft guidance.
Dr Andrew Green, chair of the GPC’s clinical and prescribing subcommittee, said NICE’s advice was likely only to benefit healthy people who visit their GP, and had an ‘opportunity cost’.
He says: ‘My concern is that if we devote a lot of effort to people who are at lower risk of heart problems, we will be unable to do the things we need to, like care for the sick, and the benefit for those at the lower limits will be low.’
But Dr Matthew Fay, a GPSI in cardiology in Bradford, argues the increased workload will be justified.
He says: ‘In my home town, Bradford, cardiovascular disease is the biggest killer. So anything that makes treatment more aggressive has got to be a good thing.
GPs face further upheaval later this month, with the Joint British Societies set to publish their third guideline, JBS3, which will recommend using ‘lifetime risk’ to prescribe statins. This would pick up additional younger people who may benefit from earlier preventive measures.
Using lifetime risk
NICE advisors rejected use of a lifetime risk calculator, saying 10-year risk was ‘more relevant to whose risk could most profitably be reduced by any interventions’.
But the chair of the JBS3 guideline group, Professor John Deanfield, director of the National Centre for Cardiovascular Prevention and Outcomes at University College London, says while he supports a lower threshold ‘in principle’, NICE is failing to address younger people with modifiable risk factors whose age means they do not reach the 10% cut-off.
He says: ‘Our approach in JBS3 is to allow the GP to assess 10-year risk, but also to look at the impact of modifying risk factors at an earlier stage, and by different approaches, including what you can achieve through lifestyle changes.’
The draft NICE guideline does not significantly alter recommendations on physical activity, alcohol and weight management, although there is additional advice on diet.
But Dr Rubin Minhas, a GPSI in cardiology in Gillingham, Kent and an adviser on the previous NICE lipid modification guidelines, says a bigger push on lifestyle change is needed.
He says: ‘Between 10% and 20% risk there should be more emphasis on physical activity and exercise in particular. CV risk has become wrapped up with lipid modification – I think next time NICE has got make this cardiovascular primary prevention guidance instead.’
What does the draft guidance say?
• Use the QRISK2 risk tool to ‘systematically’ assess CVD risk for primary prevention in all patients aged 40 to 74 years. The Framingham tool is no longer recommended.
• Offer 20mg atorvastatin to all patients aged 40 years or over with a =10% 10-year risk of CVD.
• Start statin treatment in people with established CVD with atorvastatin 80mg.
• Consider people aged 85 or older to be at risk because of age alone, rather than 75 or older as previously, because the QRISK2 score goes up to age 85.
• No need for fasting bloods for non-HDL cholesterol measures.
Source: NICE draft guideline on lipid modification, Feb 2014
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.

















