The two-week urgent cancer referral is set to be scrapped and replaced by a guarantee of a four-week target for diagnosis under proposals made by a Government taskforce aimed at boosting early diagnoses and transforming cancer survival statistics.
The NHS England-appointed Cancer Taskforce – which included input from the RCGP – said that by 2020, 95% of patients referred by their GP for cancer investigations should get a definite diagnosis of cancer, or have cancer ruled out, within four weeks of being referred.
It also called for GPs to be mandated to carry out a significant adverse event review for every emergency cancer diagnosis.
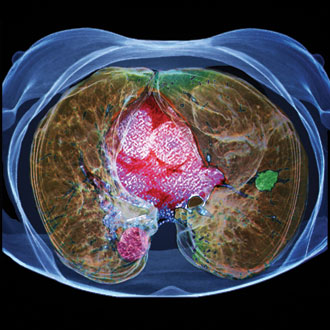
The taskforce said the NHS needs a ‘significant increase’ in diagnostic capacity – and called on NHS England to make it mandatory for all GPs to have direct access to investigations, including MRI and CT scans, by the end of this year.
It also said the new NICE guidelines for suspected cancer – which have lowered the threshold for GP referrals considerably and led to concerns practices will not be able to adhere to some of the recommendations – should be tested out in two or three ‘vanguard’ sites, to iron out any problems with their implementation.
GP leaders welcomed the report but warned the increase in diagnostic capacity would need to take place quickly and not place additional burden on GPs before they can refer patients.
The new four-week target forms a key plank of the taskforce’s five-year cancer strategy document for England, which includes measures to drive earlier diagnosis of cancer, improve communications and coordination of patients’ care and upgrade their post-treatment support, as well as ‘radically’ upgrade prevention approaches, in particular to cut smoking rates.
The report restates plans for new models of cancer pathways to ‘reduce the burden and expectation on GPs’ – including further pilots promoting patient self-referral for ‘red flag’ symptoms, whereby patients completely bypass their GP practice.
Related stories
Should patients be allowed to self-refer for cancer tests?
Patients to book own chest X-rays under new cancer self-referral pilot
Shifting the goalposts on cancer diagnosis
Cancer self-referrals made little impact on lung cancer diagnoses
NHS England unveiled plans for the new cancer strategy back in February, with a view to saving ‘at least 8,000 lives a year’ through the early diagnosis drive.
The taskforce estimates that the extra diagnostics needed to introduce the four-week diagnosis standard will cost the NHS up to an additional £300m a year by 2020, but says that by diagnosing and treating cancer earlier, and cutting down on consultant appointments through increased GP direct access, it should lead to savings of more than £450m a year.
As soon as the four-week diagnosis target is established, the taskforce says CCGs can start phasing out the two-week wait pathway.
Dr Maureen Baker, chair of the RCGP, welcomed the new four-week target, as ‘anything that can be done to lower patients’ anxiety and any undue distress when they have – or might have – cancer should be encouraged’, as well as ‘the drive to give GPs better access to relevant scanners – something that the college has long been calling for’.
However, Dr Baker warned that the system ‘is already overloaded’ and called for more diagnostic imaging and specialists to be put in place ‘before promises are made to patients that cannot be delivered’.
Dr Andrew Green, chair of the GPC’s clinical and prescribing subcommittee, said that there was ‘much to be welcomed’ in the report, including the introduction of the ‘four weeks to diagnosis’ standard.
But he warned that the GPC would not support the requirement for GPs to do significant event analyses on all emergency cancer diagnoses.
Dr Green said: ‘We cannot support compulsory significant event analysis of all cancers presenting as an emergency. I would certainly expect a GP to have a look at the patient’s notes in these circumstances, but the decision as to whether or not to proceed to a formal SEA must remain with the responsible clinician.’
Cancer Taskforce report – key recommendations
- Introduce new target for 95% of suspected cancer referrals to get a definitive cancer diagnosis, or have cancer ruled out, within four weeks of GP referral (and for 50% to get diagnosis within two weeks) by 2020.
- Mandate GP direct access to blood tests, chest X-ray, ultrasound, MRI, CT and endoscopy – by the end of 2015.
- Evaluate implementation of new NICE suspected cancer guidelines in two or three ‘vanguards’ by middle of 2016, to assess impact and ensure they are deliverable.
- From mid-2016, CCGs should let GP clinical judgement be regarded as an acceptable ‘flag’ – even if symptoms do not fit within the new NICE criteria.
- NHS England to establish national ‘diagnostic capacity implementation fund’ to help ‘unlock’ the required increase in diagnostic capacity.
- All GPs should be required to undertake a significant event analysis for any patient diagnosed with cancer as a result of an emergency admission.
- GPs be incentivised to promote faecal immunohistochemical test and bowel scope screening – to achieve 75% uptake in all CCGs by 2020.
- Public Health England to expand Be Clear on Cancer awareness campaigns.
Source: Cancer Taskforce report – Achieving world-class outcomes. A strategy for England 2015-2020
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.