1. This is a much more common problem than is often realised
Lower urinary tract symptoms (LUTS) are a common problem, especially for older men. The incidence increases with age, with up to 90% of men aged 50 to 80 years suffering potentially troublesome LUTS. The prevalence of storage symptoms increases from 3% in men aged 40 to 44 years to 42% in those aged 75 years or older. About one third of men develop urinary tract (outflow) symptoms, of which the principal underlying cause is benign prostatic hyperplasia (BPH). In my experience, once LUTS develop, symptom progression is unpredictable and varies from improving over time to rapid deterioration.
2. The most important point of history is ‘level of bother’
Men vary greatly in how they are affected by a similar level of LUTS. Some barely notice whereas others find their life becoming affected to an almost unbearable level. It is very important to enquire how much of an impact symptoms are having, as this can influence the level of treatment required, if any. It sounds obvious, but each man with LUTS has to be treated on an individual basis.
3. Remember that patterns of symptoms can direct treatment – ‘storage’ versus ‘voiding’
Always try to differentiate between storage (‘filling’) and voiding symptoms. Storage symptoms typically include urinary frequency, urgency, dysuria and nocturia. Voiding (‘obstructive’) symptoms are poor stream, hesitancy, terminal dribbling, incomplete voiding, and overflow incontinence (occurring in chronic retention). Differentiation assists in helping to provide the appropriate treatment first time round.
4. A frequency volume chart and the International Prostate Symptom Score (IPSS) are useful tools and can help clarify both the pattern of symptoms and level of bother
It is really helpful if men with bothersome LUTS have completed a urinary frequency volume chart and a validated symptom chart, such as an IPSS, before referral. It is amazing how often this can help guide management and identify unexpected behaviour. Renal function tests, such as a serum creatinine test and eGFR, should usually only be performed if renal impairment is suspected.
5. Always remember that conservative management – fluid management, bladder training and pelvic floor exercises – can be effective
For men whose LUTS are not bothersome or complicated, advise on lifestyle measures, such as moderating fluid intake – particularly in the evening – and cutting down on fluids containing alcohol, caffeine and artificial sweeteners, as well as avoiding carbonated drinks. Remember that distraction techniques, such as breathing exercises and perineal squeezing, can be helpful as part of a programme of bladder training. Make sure that any drugs that stimulate urinary frequency are kept to a minimum.
6. Medication strategy should be symptom driven. Combinations of α-blockers, α-reductase inhibitors and anticholinergics are reasonable
Offer drug treatment only to men with bothersome LUTS when conservative management
options have been unsuccessful or are not appropriate. In moderate-to-severe LUTS, offer an α-blocker, and with severe storage LUTS that are suggestive of overactive bladder, offer an anticholinergic. In mild LUTS and a prostate estimated to be larger than 30g (or a PSA greater than 1.4ng/mL and high risk of progression), try a 5-α reductase inhibitor. If the LUTS are moderate-to-severe, consider an α-blocker plus a 5-α reductase inhibitor.
Treatment should be continued for at least a period of six months. Beware the side-effects of 5-α reductase inhibitors on sexual function – patients should be warned that the resultant loss of libido and erectile function may not be recovered once the medication is discontinued. For mixed symptoms dominated by those related to storage, consider adding an anticholinergic to an α-blocker.
7. PDE5 inhibitors can be helpful in treating LUTS
PDE5 inhibitors have been identified as effective in improving LUTS, and are associated with some positive side-effects. Having previously been viewed as potentially economically unviable, the recent change of taking sildenafil off-patent has now made this a more available option. It is also worth remembering that tadalafil has a dual licence for BPH and erectile dysfunction.
8. Do not be too anxious about the risk of retention with anticholinergics
There is very little evidence to suggest any cause for concern about the risk of sudden acute urinary retention when prescribing anticholinergics – either as a single agent or in combination therapy – for men with LUTS. The most important factors in predicting which patients may develop urinary retention include patient age, prostate volume and degree of bladder outlet obstruction, and duration of symptoms.
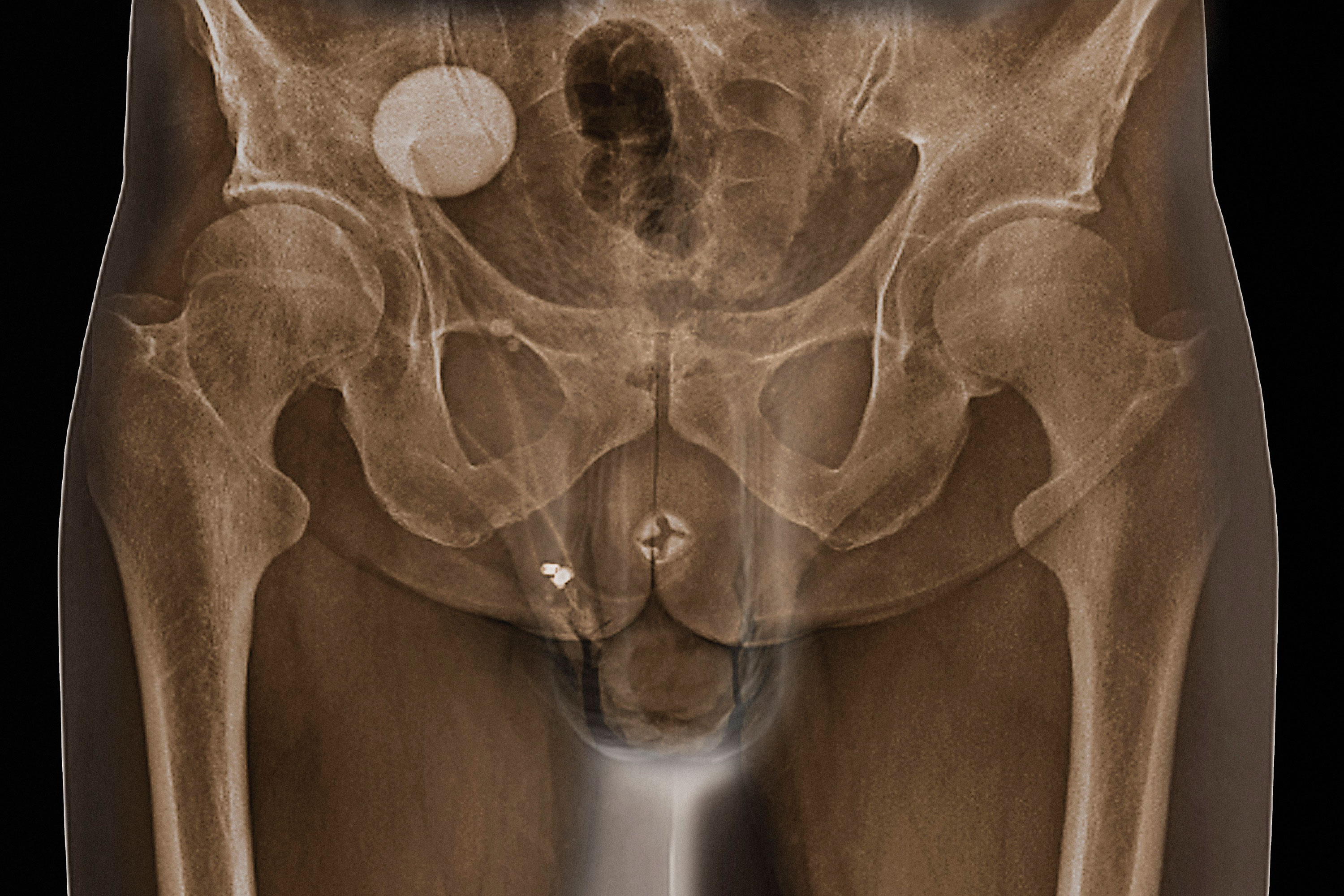
9. Should conservative management and medical therapy fail, or not be tolerated, then surgery is the next step
Men should be referred for specialist assessment if they have significantly troublesome LUTS that have not responded to conservative management or drug treatment. Other factors requiring specialist appraisal in this regard include recurrent or persistent UTIs, urinary retention, renal impairment due to lower urinary tract dysfunction and urinary incontinence.
10. Standard surgical options include TURP and Holmium laser enucleation of the prostate (HoLEP)
TURP remains the most widely available surgical option in the UK and is a very successful treatment, but it is associated with certain complications and side-effects that may put off patients, including:
• A two- or three-night inpatient stay.
• The risk of haemorrhage during surgery or after discharge.
• A prolonged recovery period before return to normal activities.
• A greater than 60% chance of dry ejaculation or a change of sensation on ejaculation.
• A small chance of deterioration in erectile function.
Although it carries a similar range of risks to TURP, HoLEP is an excellent alternative when performed by expert surgeons. The procedure does significantly reduce the risk of associated haemorrhage, particularly when it is used in a patient with a highly enlarged prostate.
The prostatic urethral lift (PUL) procedure, using the Urolift device, is an exciting alternative to standard surgical approaches that can all have the potentially deleterious effects listed above. PUL uniquely allows the option of local anaesthesia (with or without sedation), a rapid return to normal activity (within days), improvement in symptoms within a few weeks and complete preservation of all aspects of sexual function.
Mr Neil Barber is a consultant urologist at Frimley Park Hospital, Surrey
Dr Roger Henderson is a GP in Newport, Shropshire
Further reading
Perera M et al. Prostatic urethral lift improves urinary symptoms and flow while preserving sexual function for men with benign prostatic hyperplasia: a systematic review and meta-analysis. Eur Urol 2015, 67; 4: 704-13

















