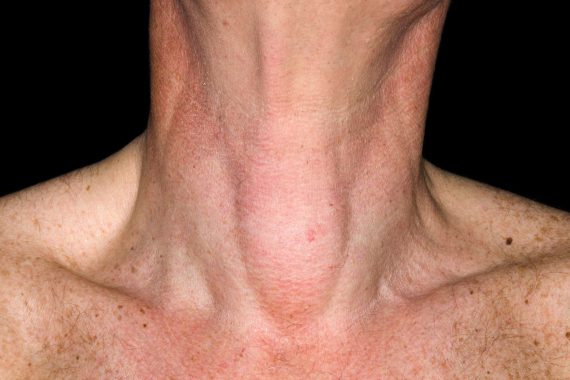
cystic nodule on the thyroid gland 3×2
1. A persistent or growing neck lump requires a diagnosis
The finding of a neck mass is a clinical sign. But it is only a sign, and it needs a careful history and possibly special investigations to be considered in establishing a diagnosis.
Neck lumps are exceptionally common but important, and serious pathologies can present with a neck mass. As a result, it is important to consider all entities when faced with a patient presenting with a neck lump.
If you are at all worried, the patient should be urgently referred for further investigations.
2. Age is helpful when dealing with a neck lump.
Age is helpful when dealing with neck lumps. On its own it is not pathognomonic, but younger patients often have benign lymphadenopathy or congenital conditions, such as branchial cysts and thyroglossal cysts. Malignant pathology such as lymphoma can occur within a paediatric setting, so all neck lumps should still be assessed and, if persistent and enlarging, be referred on for further investigation.
As age increases, the chance of malignant potential with a neck lump rises. However, this should be integrated with other risk factors in the history and examination in stratifying the malignant potential of a neck lump.
3. Site is important when dealing with a neck lump
Certain neck lumps are situated in specific areas. Midline neck lumps are commonly associated with the thyroid gland or with a thyroglossal cyst remnant. High neck lumps close to the mandible are often salivary in nature, either from the parotid or the submandibular gland, or from a branchial cyst. Unfortunately, a lymph node can also arise almost anywhere in the neck, and has to be considered in the differential diagnosis of a neck lump anywhere in the neck.
4. Refer to a neck lump or two week wait clinic
If it is felt necessary to refer a neck lump on for further diagnostics, then you should consider referral to a dedicated neck lump or two week wait referral clinic that is usually associated with an ENT service.
The only other group to think about are the children who commonly have benign lymphadenopathy, but if symptoms are concerning they can be sent to the paediatricians or dedicated paediatric ENT surgeons, who have access to a slightly different variety of radiological examinations, in addition to the ultrasound that may be more appropriate.
5. Progressive hoarseness and dysphagia are worrying symptoms
Sinister symptoms of a neck lump are associated with rapidity of growth, associated symptoms and potential nerve infiltration.
A neck lump associated with other symptoms such as progressive hoarseness, progressive dysphagia, an oral ulceration or tonsillar asymmetry, otalgia, odynophagia and association with a smoker are concerning.
Unfortunately, the two-week wait referral form has a mix of symptoms and signs that can be easily ticked, but cover a wealth of both benign and malignant potentials.
6. What investigations will the specialist want to do?
When referred to the neck lump, rapid access or two-week wait referral clinic, the specialist will want to clarify between malignant and benign pathologies.
After a careful history, fibre optic nasendoscopy – a careful oral and oropharyngeal examination – is undertaken, to look at all the mucosal surfaces where any malignant lymphadenopathy may have originated from.
The next investigation for the neck lump is an ultrasound, with or without a fine needle aspirate cytology or biopsy. This should be done by a dedicated head and neck radiologist who has a sound understanding of the pathologies in the neck. They will also have a good adequacy rate in their biopsies and will work closely with the cytopathologists, and then this information can be sent back to the surgeon running the diagnostic clinic.
There are many other tests that could be coordinated to investigate benign pathologies and also to further investigate malignant pathologies, but the careful examination of the upper aerodigestive tract and an ultrasound with or without fine needle aspiration cytology or biopsy are most important to help distinguish between benign and malignant pathology.
7. Every head and neck cancer centre should have a diagnostic rapid access urgent two-week wait referral clinic
This is an excellent resource and will have access to the necessary specialist radiology and cytology services to aid in the specialist diagnostics required. From the point of receiving the patient referral, a history, examination, and on the same day diagnostics should be undertaken within a two-week period. This reassures a patient who has a benign neck lump, and also fits the patient into the cancer pathway urgently if the neck lump is malignant.
Urgent two week wait referral clinics do also exist in stand alone ENT departments, who will refer on to a head and neck centre if something concerning is found.
8. If you’re worried, get the patient onto the cancer pathway
There are a lot of benign neck lymphadenopathy cases out there, meaning it is a difficult decision in primary care as to whether to request an ultrasound.
If you have access to the specialist radiology, it is an excellent idea to use them to reassure the patient. But if you are worried about a neck lump, it will be quicker to get the patient into the cancer pathway by referring them into the clinic, rather than delay by getting your own local ultrasound.
In my practice, any outside ultrasound performed is always repeated by our dedicated head and neck radiologist, as they can then give their opinion as well as sample the lump if appropriate.
9. Avoid biopsying a neck lump in a minor-ops clinic in primary care
Misdiagnosis and tumour spillage have poorer outcomes if surgical biopsies are undertaken in primary care. Consequently, I would suggest caution if considering a local anaesthetic excision.
I have seen supposed sebaceous cysts excised and parotid tumours or squamous cell carcinomas biopsied and spilt into a wound on more than one occasion. I have also been surprised when my radiologist has sampled a neck lump that looked benign and has turned out malignant. In this situation, I am fortuitous to have been forewarned and allowed to do further investigations before undertaking a more planned surgical approach.
10. Neck lumps seen by general surgeons are inappropriate
ENT surgeons and maxillofacial surgeons see the majority of neck lumps. Even more specialised within these groups are dedicated ENT or maxillofacial head and neck surgeons.
Lymphomas in my practice are urgently referred to the haematology and oncology team and kept within the cancer pathway. Tuberculosis is an increasing presentation in lymph nodes and is referred directly to the infectious diseases team. The infectious diseases team also picks up on any HIV-positive tests undertaken in the clinic for lymphadenopathy.
Mr Francis Vaz is a consultant ENT surgeon at University College Hospital.