The Case
A 58-year-old male accountant presents with chest pain and dysphagia that he has had for three months. He used to smoke in his twenties, but he doesn’t have a family history of any problems and he is not on any regular medication and only takes paracetamol when needed.
He completed a cardiac exercise tolerance test and this was reported as normal. An urgent gastroscopy was also reported as normal.
Oesophageal manometry showed an elevated lower oesophageal sphincter pressure of 54mmHg (the normal range is 10-45). After a wet swallow, there was a failure of complete relaxation to the gastric baseline.
Definition
The passage of food through the oesophagus is mediated by a regular and coordinated rhythm generated by the contraction of muscles that propels food forward and then into the stomach. This process can become irregular, uncoordinated and even exaggerated, resulting into oesophageal spasm and pain.
Epidemiology:
Motility disorders in the oesophagus can be the result of:
Uncoordinated contractions (diffuse oesophageal spasm)
Diffuse oesophageal spasm is the result of simultaneous uncoordinated contractions of the distal oesophageal smooth muscle. The exact aetiology is not known, but animal studies suggest that altered degradation and/or synthesis of endogenous nitric oxide (NO) is involved in the pathogenesis of the condition.
Inadequate lower oesophageal sphincter relaxation (achalasia)
The cause of achalasia is unknown and it can affect any age group. Both genders are affected equally.
Hyper contractible oesophagus (nutcracker oesophagus)
There is documented evidence that nutcracker oesophagus is associated with acid reflux. Significant acid reflux was detected on PH monitoring in patients with nutcracker oesophagus, but a study could not find sufficient evidence to suggest a relationship between nutcracker oesophagus and acid reflux.¹ Even so, you should still be very aware of the significance of acid reflux on quality of life and the importance of treatment.¹
Clinical Features
Oesophageal spasm is a common cause of non-cardiac chest pain. It affects about 25% of the population during their lifetime and accounts for 3-10% of presentations to hospital accident and emergency departments.
Oesophageal dysmotility disorders can be secondary to other conditions:
- Scleroderma
- Multiple sclerosis
- Lesions
- Stroke patients
Uncoordinated contractions (diffuse oesophageal spasm)
Around 10% of patients presenting with non-cardiac chest pain have diffuse oesophageal spasm. 3-5% of patients with diffuse oesophageal spasm develop achalasia.
Symptoms for diffuse oesophageal spasm can range from non-specific chest pain and dysphagia to gastro-oesophageal reflux disease. The symptoms can last from seconds to minutes or even longer. Symptoms can be initiated by ingestion of food or drink, but they can also present independently.
Pain due to oesophageal contractions may be caused by retention of food bolus causing oesophageal distention. This may result in pain due to a massive increase in oesophageal muscle wall tension; if prolonged this can potentially cause muscle wall ischaemia in the oesophagus. In addition, hypersensitivity to oesophageal distension and contractions may contribute to symptom generation.
Psychiatric conditions such as depression are a common finding in these patients and should not be left untreated. The symptoms associated with eating can result into nutritional insufficiency which can worsen the depressive disorder.
Inadequate lower oesophageal sphincter relaxation (achalasia)
The main symptom is dysphagia with 100% to solids and about 75% to liquids, but this can fluctuate. Cough and chest infection can develop secondary to aspiration of pooled oesophageal content. There is a slight increase risk of developing squamous cell carcinoma of the oesophagus.
Hyper-contractible oesophagus (nutcracker oesophagus)
It is one of the most frequent oesophageal motor disorders in patients with non-cardiac chest pain.
One study concluded that nutcracker oesophagus was associated with chest pain and dysphagia.2
Differential diagnosis
Differential diagnosis include:
- Tumours
- Oesophageal web
- Schatzki ring
- Constricting-oesophageal mass
- Extra-oesophageal mass
- Benign strictures due to gastro-oesophageal reflux disease
- Neural plexus infiltration by tumours
- Cardiac chest pain
- Biliary colic
- Pancreatic pathology
How GPs diagnose this with certainty?
Uncoordinated contractions (diffuse oesophageal spasm)
A trial of acid suppression in a patient with no red flags can be beneficial in distinguishing GORD from other causes. Investigation for oesophageal spasm is often not the first choice as exclusion of cardiac chest pain and malignancy is often the primary aim of physicians.
Oesophageal manometry is the gold standard for the diagnosis of diffuse oesophageal spasm. Manometry has shown that more than 30% of wet swallows have simultaneous contractions.
Inadequate low oesophageal sphincter relaxation (achalasia)
Gastroscopy may not be diagnostic, but can show a dilated oesophagus with food and debris. Barium swallow can be helpful in demonstrating a narrow and tight lower aspect of the oesophagus with a dilated proximal segment.
Oesophageal manometry is a very useful investigation demonstrating a prolonged contraction in the lower oesophageal sphincter.
Hyper-contractible oesophagus (nutcracker oesophagus)
Dysphagia may be to both solids and liquids and can cause chest pain, but it may also be asymptomatic.
On oesophageal manometry, the contraction in the oesophagus follows a normal propagation, but the amplitude and duration of contraction is highly elevated. Contractions can have a pressure exceeding 180mmHg. It is one of the most frequent oesophageal motor disorders in patients with non-cardiac chest pain.
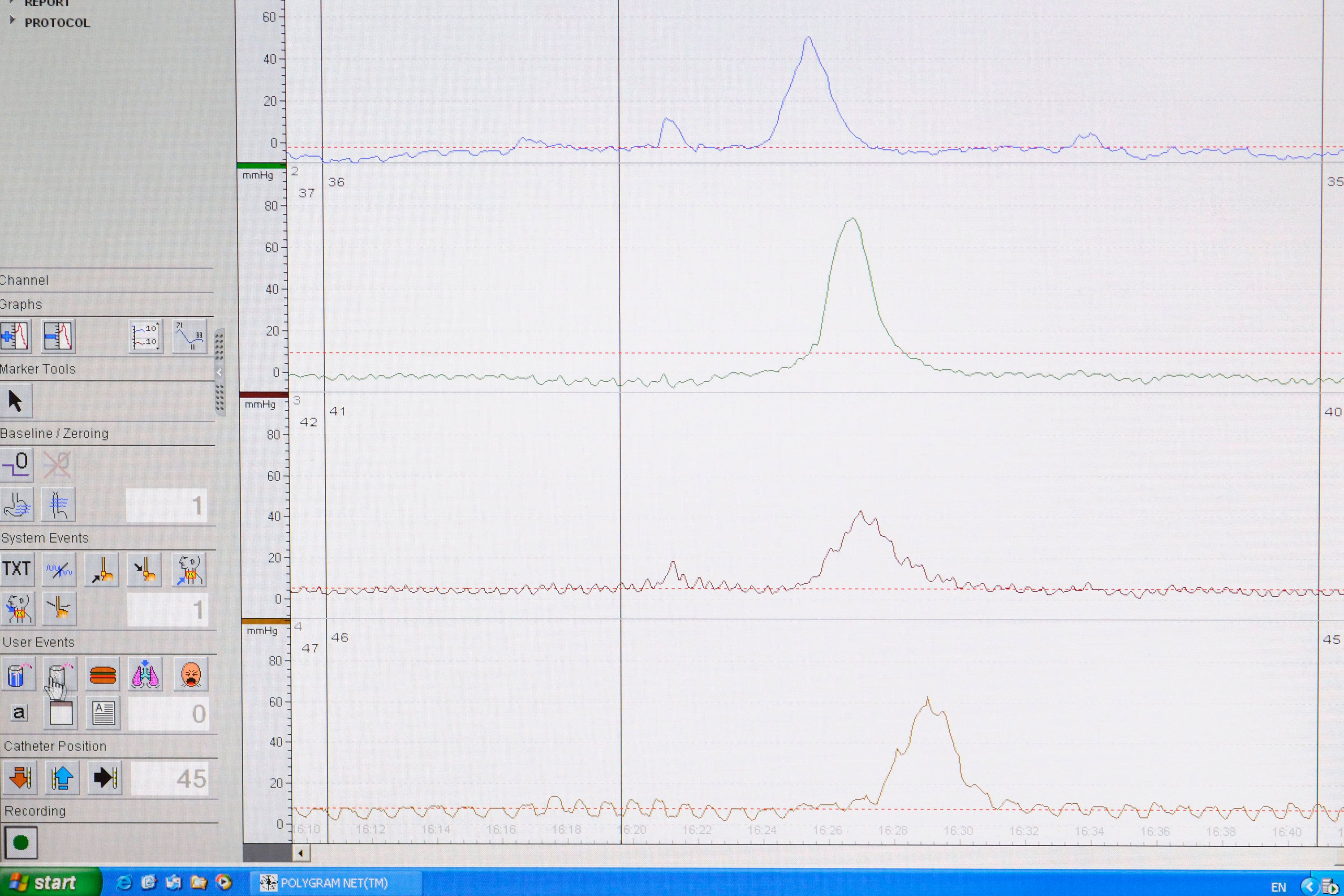
oesophageal manometry and p h testing spl suo 3×2
Treatment
Uncoordinated contractions (diffuse oesophageal spasm)
Initially lifestyle modifications should be considered as many of these factors can be very contributory to the symptoms and therefore simple modification in eating habits, exercise, and stress reduction can be invaluable.
Non-pharmacological treatment includes warm water and peppermint oil.
Smooth muscle relaxants and antispasmodics have been shown to have positive effects on symptoms when used either prophylactically or when symptoms are present.
Inadequate low oesophageal sphincter relaxation (achalasia)
Medical treatment for inadequate lower-oesophageal sphincter relaxation includes nitrate-based drugs such as isosorbide mononitrate (ISMN), sildenafil and calcium-channel blockers such as nifedipine.
Botulinum-toxin injection at the gastro-oesophageal junction during endoscopy is beneficial, but the therapeutic effect will wear off after a while, resulting in the need for repeated therapies. Antibodies can develop to the botulinum toxin and can weaken the effect of therapy. Pneumatic dilatation of the lower-oesophageal sphincter has 60-90% response rate with a 3% perforation risk and a 0.5% mortality rate.
Surgical myotomy has a 90% response rate and the longest response rate. Half of these patients will require acid suppression for gastro-oesophageal reflux disease. Recent advances in endoscopic therapy have allowed endoscopic myotomy, which currently takes place in specialised centres under skilled endoscopists. This is certainly the future for the treatment of achalasia as it avoids the need for surgery and reduces the need to stay in hospital.
Hyper-contractible oesophagus (nutcracker oesophagus)
Non-pharmacological treatments are similar to that of diffuse oesophageal spasm and include using warm water and peppermint oil. Diltiazem, nitrates, sildenafil and antidepressants have shown to be beneficial too.
Dr Durayd Alzoubaidi is a clinical research fellow and gastroenterology SpR at University College London Hospital.
Dr Rehan Haidry is a consultant gastroenterologist and endoscopist at University College London Hospital.
References
- M. Borjesson, P. Rolny, C. Mannheimer, M. Pilhall. Nutcracker oesophagus: a double-blind, placebo-controlled, cross-over study of the effects of lansoprazole. Aliment Pharmacol Ther, 18 (2003), pp. 1129–1135
- Fornari F., Farré R., van Malenstein H., et al. Nutcracker oesophagus: association with chest pain and dysphagia controlling for gastro-oesophageal reflux. Dig Liver Dis. 2008 Sep;40(9):717-22.

















