A 51-year-old lady presented to her GP with a two week history of episodes of unilateral severe headaches associated with nausea and visual disturbances in the form of ‘jagged edges’. She described her headaches as pressure-like, each episode lasting a few hours, and was experiencing 2-3 attacks per week. These were similar to her migraines which she used to have many years ago. She believed that they were triggered by a root canal treatment she had recently.
As the general neurological examination, including fundoscopy, was unremarkable, she was reassured and was given some strong analgesics and advised to return if needed.
She returned a few weeks later as the headaches were getting more intense and lasting longer, and she was starting to feel more depressed. She had been having hot flushes for sometime and her last menstrual period was over a year ago.
Once more she was reassured and was told that all these symptoms are related to the menopause. She was prescribed sumatriptan to use with the attacks and was given regular propranolol as a prophylactic medication.
A few weeks later her neighbour contacted the surgery concerned about her. She reported that although the patient was not having the severe migraines any more, she was experiencing a constant dull headache and that she was spending most of the day in bed with the curtains continuously drown. Her daughter also reported that she was not being herself and simple household tasks were a problem to complete. She was also becoming increasingly vague and disinterested.
On assessment she reported a constant feeling of light-headiness, nausea and loss of appetite, and on examination the tendon reflexes on the left were brisk.
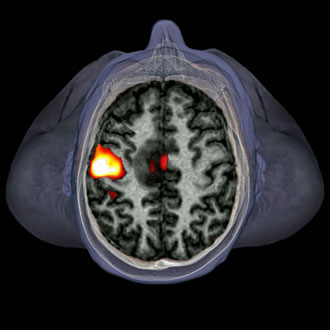
The GP managed to arrange an urgent brain CT scan the next day. It showed a large enhancing lesion in the inferior right frontal lobe with midline extension. There was significant surrounding oedema resulting in effacement of the sulci, right lateral ventricle and a degree of the sub-falacine herniation.
She was admitted directly from the radiology department to the neurosurgical unit where she had craniotomy and debulking of what was found to be glioblastoma multiforme (GBM – WHO grade IV)
The problem
Headache has a lifetime prevalence of 96%. It is one of the most common presentations in general practice and nearly 30% of referrals to neurology are headache-related.1, 2
Migraine affects 15% of the UK adult population and 80% have episodic tension-type headaches.3 Migraine is characterised by episodes of severe headaches associated with nausea, vomiting and sensitivity to light, sounds and odours. 20-30% of migraines are also associated with a temporary neurological deficit (aura) lasting up to one hour. These are usually visual, sensory or speech related and very rarely can be motor. 3, 4, 5
Migraine affects one in four women and one in 12 men, with the tendency to get worse at the perimenopause-menopause phase of women’s lives before it gets better.5
Although depression and other mental illnesses are common in migraines sufferers6, worsening symptoms with a progressive, new-onset headache should always be taken seriously.
Features
GBM, although the most common and most aggressive of the malignant primary brain tumours in adults, is rare with an incidence of two to three per 100,000 people in Europe and the United States. It usually presents with sub-acute and progressive nausea, vomiting, neurological deficit, change in personality, forgetfulness, confusion, headaches, seizures and later on coma and death due to cerebral oedema.7
Diagnosis
Always keep an open mind and assess for the rare and sinister causes of headaches. Urgent referral to a neurologist should be sought for further investigations if suspected.
The red flag features that should prompt referral are: 3, 4
• New or unexpected headache in over 50 years.
• Progressive, worsening headaches over a few weeks.
• Thunderclap, or abrupt and explosive headaches – same day assessment.
• Migraine-like with atypical aura lasting less than five minutes or more than one hour.
• Headache that changes with posture.
• Headaches precipitated by physical exertion or Valsalva manoeuvre e.g. coughing, laughing.
• Jaw claudication or visual disturbance.
• Abnormal neurological examination.
• Non-focal neurological symptoms e.g. cognitive disturbance.
• Headaches associated with temperature, rash, meningism etc.
• New onset headache in patient with cancer or who are immuno-compromised.
Management
Following surgery, she was treated with radical radiotherapy (60Gy in 30#) and concomitant temozolomide and bevacizumab. The survival rate of GBM is three months if untreated and 1-2 years with treatment from diagnosis.7
This patient lived for two-and-a-half years from the point of diagnosis, which was very much appreciated by the family and friends.
Dr Nassif Mansour is a GPSI in neurology and headache disorders in Surrey and a member of the Primary Care Neurology Society.
This article was commissioned with the Primary Care Neurology Society. Their mission is to support provision of neurology education and information across primary care in order to improve delivery of care to people with neurological conditions. For just £45, you can access a range of resources from www.p-cns.org.uk, including free access to Europe’s leading online neurosciences e-learning resource, E-Brain.
References
- Fuller G, Kaye C. Headaches. BMJ, 2007; 334 (7587): 254-256
- MacGregor EA, Steiner TJ, Davies PTG. Guidelines for all healthcare professionals in the diagnosis and management of migraine, tension-type, cluster and medication-overuse headache. British Association for the Study of Headache, 2010
- NICE. CG150: Headaches – diagnosis and management of headaches in young people and adults, 2012
- Beithon J, Gallenberg M, Johnson K et al. Health care guideline: diagnosis and treatment of headache. Institute for Clinical Systems Improvement, 2010
- Goadsby PJ, Lipton RB, Ferrari MD. Migraine – current understanding and treatment. New England Journal of Medicine, 2002; 346 (4): 257-270
- NICE. CG91: The treatment and management of depression in adults with a chronic physical health problem, 2009
- Johnson DR, O’Neill BP. Glioblastoma survival in the United States before and during the temozolomide era. Journal of neuro-oncology, 2012; 107 (2): 359–364