1. PCOS presentation varies across the life span.
Hyperandrogenic features are often most prominent among adolescents, while fertility issues are most prominent among women in their 20s and 30s. Metabolic challenges most notable after this.1,2
The propensity to weight gain and psychological challenges affect all ages, and metabolic features can occur early, especially among those who are overweight. Variations across ethnic groups should also be noted, such as fewer hyperandrogenic dermatological features and more severe metabolic features in Asian women, even without weight gain.
2. Know the diagnostic criteria
Diagnosis of PCOS is now largely based on the Rotterdam criteria, and requires two of three key features to confirm PCOS:3
- Oligo- or anovulation – cycles under 21 days, or over 35 days, indicate anovulation
- Clinical and/or biochemical hyperandrogenism – clinical hyperandrogenism includes hirsutism and acne, biochemical hyperandrogenism is determined through free testosterone levels
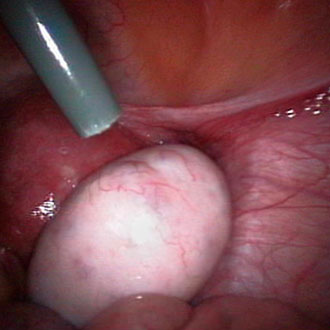
- Polycystic ovaries on ultrasound and exclusion of other aetiologies
Investigations must exclude other causes. These include:
- TFTs.
- Prolactin.
- Follicle stimulating and luteinising hormone – FSH and LH levels (particularly if premature menopause is suspected)
3. Vaginal ultrasound should be reserved for sexually active women
Vaginal or abdominal ultrasound is often needed for diagnosis where anovulation and hyperandrogenism are not both clearly present, but vaginal ultrasound should be reserved for sexually active women. The role of ultrasound remains controversial for adolescents, among whom a polycystic appearance of the ovaries is very common, potentially leading to over diagnosis.4
4. It is important to address psychological factors initially in women with PCOS
Prevalence of depression in women with PCOS is 28-64%, significantly higher than in the general population (around 7.1-8%), while the prevalence of anxiety ranges from 34-57%.5 Therefore screening, assessment and treatment of depression and anxiety are vital and should be routinely screened for.
Eating disorders, negative body image, low self-esteem and psychosexual dysfunction should also be considered, as these are all more common among women with PCOS.
5. Lifestyle change should be first-line therapy for all women with PCOS
This should focus on support and education, ensuring that patients understand the link between insulin resistance and obesity in PCOS and the importance of prevention of weight gain.
Among those who are already overweight, multidisciplinary lifestyle intervention aimed at improving insulin resistance and aiding weight management needs to be strongly emphasised.
6. A weight loss of 5-10% will greatly assist in symptom control in overweight patients
Modest weight loss of 5%–10% of initial body weight significantly reduces insulin resistance and has been demonstrated to improve many of the features of PCOS, such as abdominal fat, hyperandrogenism, abnormal lipids, anovulation, menstrual irregularity, subfertility, and all risk factors for diabetes and cardiovascular disease.6
There are no specific diets found to be favourable over another, so the focus should be on calorific restriction. Encouraging 30 minutes of moderate to vigorous exercise daily is also required for health goals – this will not reduce weight alone, but increased opportunistic movement has significant health benefits.
7. Women with PCOS are a population at high risk of developing diabetes and cardiovascular disease
This is due to an increased prevalence of metabolic syndrome, which increases cardiovascular risk factors as a consequence of hyperinsulinaemia, dyslipidaemia, and hypertension. There is a 5–10-fold risk of progression from pre-diabetes to diabetes and a 4–8-fold risk of developing diabetes.7
It is also important to note that relatives of women with PCOS may have increased risk of diabetes and increased CVD risk factors.
Metabolic features are often poorly appreciated in PCOS, hence, recommendations on screening and assessment of diabetes and cardiovascular risk factors is important. Your assessment should include:
- Age
- Weight
- BMI
- Waist circumference
- Smoking history
- Lipid profile
- Blood pressure
- Glycaemic status
8. Fertility is not necessarily impaired in all PCOS cases
Some women conceive without medical intervention, depending on the severity of the condition. Age and BMI have a critical role in infertility risk in PCOS. Fertility rates are lower among women with a BMI of 30-32, and so maintaining a BMI under 30 is ideal for increasing the chance of conceiving.
9. Metformin can be started before referral for clomiphene
Clomiphene is the first-line pharmacological therapy, but in primary care metformin can be started before specialist referral for clomiphene. Clomiphene treatment should be accompanied by follicle tracking to minimise the risk of multiple pregnancy.
Metformin improves ovulation, re-establishes cycles, reduces insulin resistance and reduces progression to diabetes. It may prevent weight gain but does not induce weight loss. You can minimise the side effects by starting with a dose of 1 x 500mg daily, and increase by 500mg per fortnight up to a 1500mg-2000mg average dose.
10. Cyproterone acetate-containing pills are best for acne and hirsutism
Cyproterone acetate-containing pills are more advantageous in reducing acne and hirsutism due to their central effects action – reducing the production of ovarian androgens and the amount of free testosterone in circulation – and act locally at the skin level by antagonising the effects of androgens, competing with them for the nuclear androgen receptors.
Dr Marie Gerval is a clinical research fellow in endocrine gynaecology at Chelsea and Westminster Hospitals NHS Foundation Trust, and Imperial College London.
Mr Nick Panay is a consultant gynaecologist at Chelsea and Westminster Hospitals NHS Foundation Trust.
References
- Moran L, Gibson-Helm M, Teede H, Deeks A. Polycystic ovary syndrome: a biopsychosocial understanding in young women to improve knowledge and treatment options. J Psychosom Obstet Gynaecol, 2010;31(1):24-31
- Moran LJ, Misso ML, Wild RA, Norman RJ. Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update, 2010;16(4):347-363
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril, 2004;81(1):19-25
- Kristensen S, Ramlau-Hansen C, Ernst E, et al. A very large proportion of young Danish women have polycystic ovaries: is a revision of the Rotterdam criteria needed? Hum Reprod, 2010;25(12):3117-3122
- Deeks A, Gibson-Helm M, Teede H. Anxiety and depression in polycystic ovary syndrome: a comprehensive investigation. Fertil Steril, 2010;93(7):2421-2423
- Moran L, Pasquali R, Teede H, et al. Treatment of obesity in polycystic ovary syndrome: a position statement of the Androgen Excess and Polycystic Ovary Syndrome Society. Fertil Steril, 2009;92(6):1966-1982
- Cussons A, Watts G, Burke V, et al. Cardiometabolic risk in polycystic ovary syndrome: a comparison of different approaches to defining the metabolic syndrome. Hum Reprod, 2008;23(10):2352-2358