Welsh royal colleges have launched their ‘Choosing Wisely’ initiative, giving GPs and other doctors a list of procedures and treatments they should avoid in order to help minimise harm from unnecessary healthcare interventions.
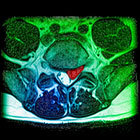
The Academy of Medical Royal Colleges (AMRC) in Wales has told GPs to avoid X-rays or scans in patients with lower back pain and prescribing medicines to frail people in their last year of life except for the control of symptoms.
The initiative was announced by the UK AMRC last year. As part of the scheme, each of the medical royal colleges was invited to come up with a list of around five treatments or investigations that doctors should avoid doing.
Unveiling the programme in Wales, the AMRC said it wants to ‘embed a broad cultural change in healthcare where clinicians and patients regularly discuss the value of treatments and make shared decisions’.
The programme also encourages GPs to get patients to ask questions about their care – and provide them with a leaflet suggesting the four key questions: ‘What are my options?’; ‘What are the benefits and harms?’; ‘Do I really need this?’; and ‘What can I do to help myself?’.
Of the final list of treatments and tests to avoid, the Wales programme is asking GPs to avoid:
- X-rays or scans in people with low back pain;
- long-term prescriptions for PPIs;
- prescribing medicines to frail people in their last year of life except for the control of symptoms;
- checking cholesterol levels every year if they are taking a statin, unless they have a history of vascular disease or an inherited lipid disorder.
It also calls for GPs to make sure healthy people are properly involved in choosing to start taking a preventive medication for heart disease or osteoporosis.
In addition, the RCGP says patients should only be considered for treatment with antihypertensive drugs if they have blood pressures of 140-159/90-99 mmHg and other risk factors, and women should always be offered hormone testing before investigating the possibility of polycystic ovary syndrome.
Dr Paul Myres, programme leader and chair of AMRC Wales, who is also a former GP in Wrexham, told Pulse the campaign was about ‘rebalancing the conversations that GPs have with their patients’.
Dr Myres said: ‘We’re looking for patients to be a bit more confident in asking what choices are available to them and for clinicians to be more confident about talking about options and not just saying this is what you should do.’
Of the RCGP recommendations, Dr Myres said that the call to only treat hypertension at above 140/90 mmHg and in patients with other risk factors related to a hangover from earlier guidelines with lower target blood pressures, which meant some patients and GPs still pursue treatment at lower blood pressure levels than this, when lifestyle changes would be more appropriate.
He said the overall message was in line ‘with the overdiagnosis movement, that more is not necessarily better and to look for alternatives’.
But he stressed that although there could be advantages for the NHS in terms of reduced waste and lost opportunity costs, the programme was ‘not about saving money’.
Dr Myres said: ‘We’re not expecting every GP to suddenly work on all five and we recognise that certainly in Wales, local groups may choose to focus on certain ones. What we’re very keen to avoid is for CCGs – or here in Wales, the local health boards – to focus on key areas because what we hear very clearly from patients is that this is about saving money.
‘It’s not about saving money it’s about safety and effectiveness and avoiding waste.’