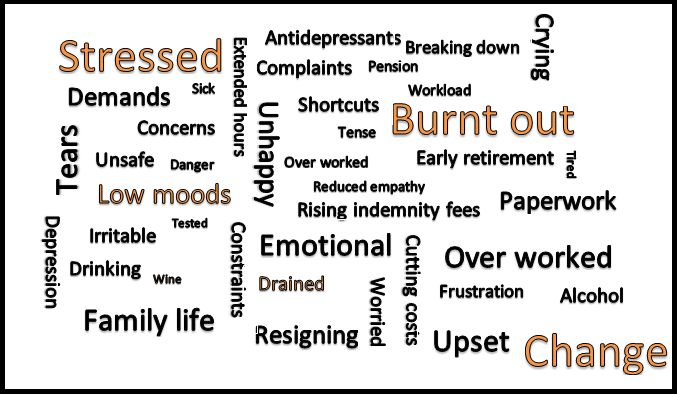
buzzword image
Struggling to care
‘I realised I was suffering from burnout when a lady who was going through a really awful situation and who had seen me a few times about it came with even more bad news, distressed, crying and saying she did not think she wanted to live anymore. My only reaction was to resent her for coming to see me and taking up so much of my time.’
‘Sometimes find it difficult to really empathise with patients. Just look at them as one more hurdle in the race to finish surgery and tackle the next task.’
I care less: not careless or not caring, but just “care less”
‘Sheer volume of work is making me less sympathetic at the end of the day, and after a full day on duty I still have to offer an Extended hours routine surgery from 6.30 to 7.30pm for working patients. I am not the best GP I could be at this time.’
‘Reduced empathy at times, and at times seeing patients as a burden. One common theme when discussing with my colleagues that that when a complex or ill patient comes in, a gut reaction can be “Oh no, this is going to take ages” because of the pressure on time, even though it may be the only person who really needs to see you that clinic.’
‘When I was suffering from burnout in 2014 and early 2015, I reached a point where I didn’t really care about the wellbeing of my patients, because I was so utterly drained and exhausted. This caused me to be less patient and considerate to them, particularly the complex, demanding and difficult ones.’
‘I care less: not careless or not caring, but just “care less”.’
‘Compassion fatigue. Lack of time to adequately deal with patients’ emotional needs. Having to see patients on my days off and own time for this eg at end of a surgery.’
Turning to alcohol and prescription drugs
‘I notice that I am dreading my working days, and occasionally even dread calling in my patients when I am at work. When I feel tense before a day of work, I sometimes drink alcohol to ease the stress and remain calm at home. I am aware of this, and try to not drink over the recommended 14 units per week. But I am worried for the reasons I have a glass of wine, as it is not simply for enjoyment, but used as a way to deal with stress.’
I drink a bottle of wine most evenings after work, and often take codeine to help me get to sleep
‘For some time I have kept a supply of “beta blocker” tablets at hand in my consulting room. I often find myself reaching for one. They help stop the palpitations, tremors and sweats which I get when I am stressed. I did consider taking antidepressants but those are better for low mood not acute stress symptoms. Retirement is in my mind almost every day. What stops me is that I still enjoy the work – sometimes – and I feel my patients need experienced GPs, so I am carrying on for a while yet.’
‘I had to go onto antidepressants when I started suffering with burnout in 2013/14, and I remain on quite a high dose (20mg Escitalopram) otherwise I find that I get overwhelmed at work. I have also been unable to return to my job as a GP partner and now locum very part time.’
‘I drink a bottle of wine most evenings after work, and often take codeine to help me get to sleep. I am also on long-term antidepressants, as are a lot of my colleagues.’
‘I was drinking to excess in the evenings and this caused a marriage breakdown. I tackled this with help of family and I now only have alcohol on special occasions, I would not say I was an alcoholic but it could easily have gone that way as I was using alcohol to relieve the stress. I was then prescribed antidepressants by my GP which I still take now. I’ve handed my resignation into my partnership and I hope to do more locum-type work when my notice period ends in March next year.’
Negative perceptions
‘The “pointless crap” gets me down as does the workload and the persistent negative press. I find the on call days can be awful, that’s the really stressy/ burnout part. I feel the future of general practice is very depressing. The government seem to feel we can be replaced with a nurse practitioner or an app, well good luck with that and when secondary care is drowning it will be too late.’
‘I am completely sick of it. No one pays me any more for seeing what once would have been entire day’s patients in a single morning clinic. I just get the pleasure of dealing with more complaints and rising indemnity fees. In fact my pay was effectively cut by 2.2% in June when my indemnity fees went up 12% this year. I pay the fees out of my own salary and it costs me £680 a month for doing 2 1/2 days a week. My practice refused to cover the cost.’
Unsafe care
‘I have a feeling that I am working within an entire system which is unsafe, where the workload pressures have long since exceeded capacity, and where the basic infrastructure is so degraded that it makes my job more difficult, rather than easier.’
I am completely sick of it.
‘I am surrounded by constraints on investigating, referring and managing patients that cripple my ability to function. I can no longer rely on the rest of the system to counteract any errors I might make, and indeed the rest of the system seems to be making numerous errors.’
‘It takes a lot of concentration to carry out our job, particularly with increased comorbidity and complexity. I find it a struggle to spot patterns emerging and hence get a definitive diagnosis. As a result I’ve scaled down my out-of-hours commitment to spare myself for the day job.’
The personal effect
‘I didn’t realise how bad it was until I snapped and shouted at a member of staff, then broke down in tears at partner meeting when discussed. I took two weeks off and had planmed to reduce sessions at the surgery, but realised that wasn’t enough for me. I no longer wanted to be at the surgery I had originally planned to retire from and so instead resigned and found a new practice.’
‘Personally, I find the worry at the end of the day and sleeplessness most troublesome because I have been too busy and the day is a blur.’
If you are worried about your health, then you are able to access free counselling in England from the GP Health Service. Click here for more details.

















