
General practice has been undergoing a quiet revolution in recent years that has had little fanfare: it is now an overwhelmingly part-time profession.
Official figures suggest almost 70% of the workforce work less than full time in general practice – the highest proportion ever.
There are huge caveats. Many GPs counted as less-than-full-time (LTFT) workers – defined as those working less than 37.5 hours a week – do more hours in reality than other professionals working full time. And in many cases, they are doing other healthcare-related roles outside general practice.
But the figures reveal a powerful truth for the profession – that the vast majority of GPs are revolting against working 60-plus hour weeks in general practice and are voting with their feet.
Young and old GPs are turning to salaried roles with more clearly defined sessions, and in many cases to locum work, in a bid to restore flexibility and control to their working lives – control lost as a result of ministers’ continued neglect of the profession.
Hull GP Dr Zoe Norris, chair of the BMA’s GP sessional subcommittee, says it is ‘inevitable’ that LTFT working will be the future of general practice.
‘It seemed to come as a shock a few years ago when suddenly people started reducing their hours, largely because of a predominance of women, but now we’re also seeing that in our male colleagues because they want to have a life outside of medicine too.
‘That’s okay and normal. It’s the only way to make the job manageable.’
The figures bear this out. Female salaried GPs are still more likely to work less than full time – 91% do so now – but three-quarters of male salaried GPs do likewise, up from 71% in September 2015.
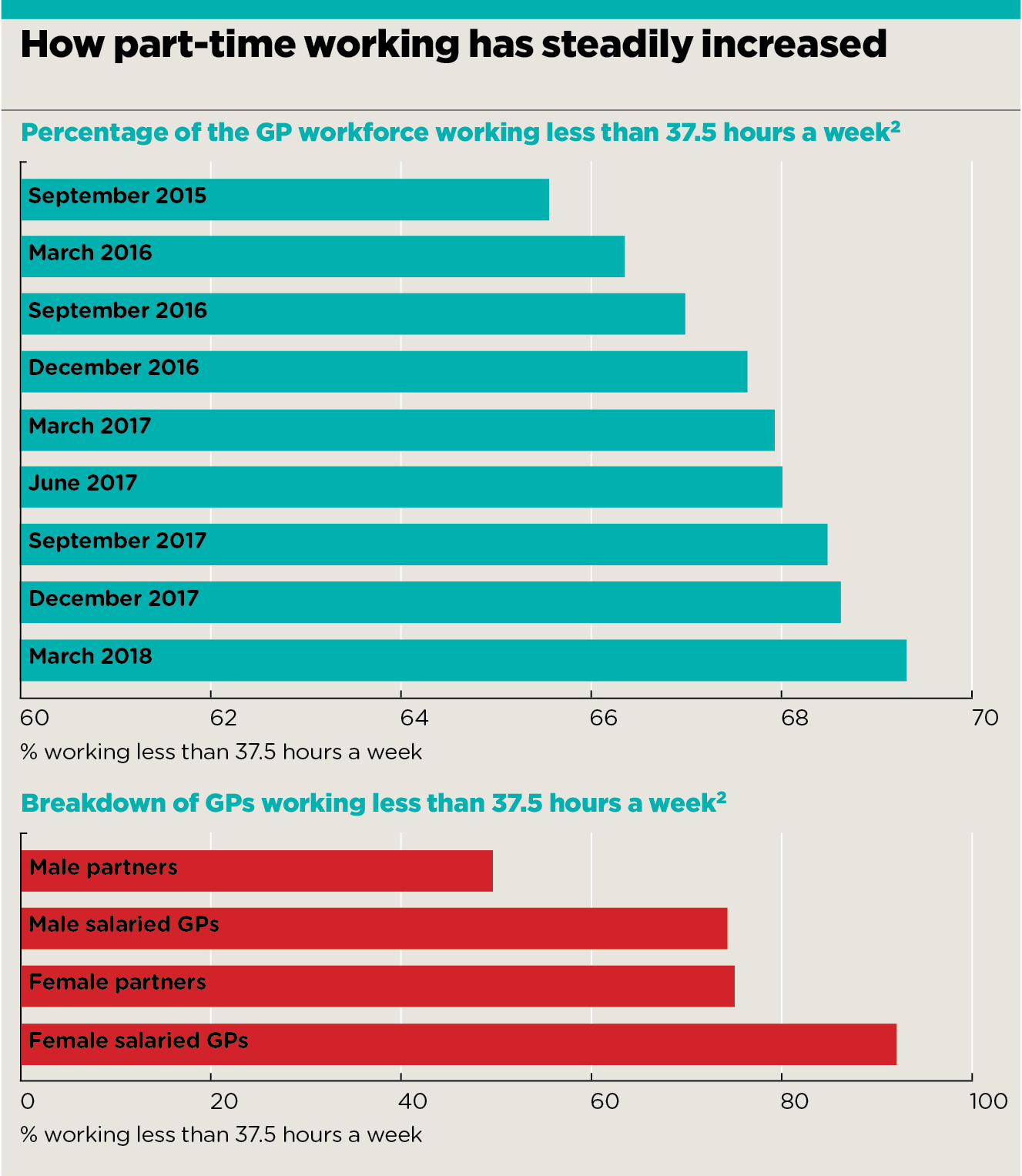
p9 cover feature graphs
And leaders are waking up to the fact GPs are changing, and the profession needs to find ways to adapt. The landmark partnership review – led by Wessex LMCs chief executive and GPC member Dr Nigel Watson – published its interim report last month. It advocated a move towards ‘primary care networks’ to offer more flexible working, and suggested drawing on elements of locum working.
Meanwhile, even health secretary Matt Hancock has highlighted that the flexibility of general practice is ‘attractive’ to the younger generation, while both NHS England and Health Education England have started actively promoting this aspect of the profession. This is making a difference – record numbers of medical graduates are entering GP training, it was announced last month.
Of course, ‘part time’ is a relative concept. Dr Matt Mayer, chief executive of Berkshire, Buckinghamshire and Oxfordshire LMCs, says the term is a ‘misnomer’ because GPs working three days a week are still ‘actually doing 14-hour days – that’s full time’.
Yet it is true that the increase in the LTFT figures shows that fewer GPs are now willing to work backbreaking hours in permanent salaried or partnership roles – even if the workload for those at the top end of the scale has increased.
It is unsustainable and unsafe to be doing full-time general practice
Dr Zoe Norris
The percentage of partners and salaried GPs working less than full time has steadily increased from 66% to 69% over the past three years. At the same time, the percentage of the GP workforce working as locums is rising, according to official data.
‘GPs are having to go “part time” in order to sustain themselves professionally and avoid burnout,’ says Dr Mayer. ‘The alternative is working five 14-hour days a week and then going off long-term sick and never coming back.’
Dr Norris agrees: ‘It is unsustainable and unsafe to be doing full-time general practice, regardless of your contractual status, and so you have to find a way for that to be sustainable. That’s usually going part time, reducing the high-pressure clinical workload and developing a portfolio career, or managing the workload by being a locum and doing a portfolio career that way.’
This is a change that has been acknowledged by the partnership review, which has come out strongly in favour of primary care networks – the large-scale organisations that will ‘involve health and social care professionals working together as a locally based, multidisciplinary teams’.
The review found 5,000 practices have already formed networks, which promise to ‘support general practice in terms of workload’, making the profession ‘more resilient and a better place to work’.
Dr Watson says the networks ‘will allow more support for individual GPs and practices and also offer opportunities for GPs to work in portfolio roles’.
Developing portfolio roles… not only improves the quality of care but GPs enjoy the variety
Dr Nigel Watson
‘A GP in my practice has an interest in diabetes. He does three days a week as a partner, a day a week doing diabetes research and a day a week doing diabetes in the community delivering care to patients,’ Dr Watson says. ‘It’s developing roles like that; it not only improves the quality of care, but he really enjoys that variety.’
Dr Watson’s review suggests other ways to help the profession adapt to the growing part-time workforce, including incorporating the flexible elements of locum working into the partnership model. The interim report says this will attract some of the locum GP workforce back into substantive posts – which is essential for the future of the profession.
Dr Watson tells Pulse: ‘Younger GPs who are not becoming partners straight away and becoming locums swells the locum number but doesn’t help the long-term sustainability of general practice.’
As a result, his review team wants to increase the number of GP partners by ‘making partnerships more attractive than being a locum’ through introducing ‘greater flexibility, improved work-life balance and portfolio working opportunities for partners’ – although the interim report has few concrete proposals on how to achieve this at this stage.
But results from Pulse’s first-ever locum survey lay bare the extent of the task ahead for Dr Watson – the majority of respondents say nothing would tempt them back to partnership.
Regardless of the outcome of the partnership review, the shift to LTFT working does have a potential casualty – the loss of continuity of care.
However, Dr Norris says the shift is inevitable and the loss of traditional continuity of care is the trade-off that will allow GPs to take workload ‘into our own hands’. The emphasis on continuity of care, she says, ‘kind of implies you can’t do a good job if you see someone as a one-off. That’s not the case’.
She adds that, instead of mourning continuity of care, GPs need to ‘get our heads round the fact we are working in bigger teams with different people… we need to make sure our handovers are better, that our notes are better and that we have clear plans’.
The trade-off is making the profession a more attractive proposition for medical graduates, she says. ‘One of the things we don’t sell is the flexibility and how brilliant general practice can be for doing different things and portfolio working. I think a lot of medical students and newly qualified GPs are excited by doing a mix of different things and by doing things other than nine sessions of face-to-face general practice in a partnership.’
Mr Hancock seems to acknowledge this. Speaking to Pulse at last month’s Best Practice Conference in Birmingham, he said: ‘Part-time GPs have always had an enormously important role and the flexibility that can come with being a GP is very attractive to many people.’
Dr Tom Micklewright, outgoing BMA GP trainees spokesperson, says the message is getting across, ‘not just that you can work part time but that general practice offers more flexible options’.
He says: ‘The new Health Education England recruitment video focuses on general practice that you can do in different areas, such as working in sports medicine or expedition and outdoors medicine – all potential career avenues.
‘I think the new generation of medical graduates are seeing GPs with a varied career portfolio and they’re thinking that looks like a very attractive career.’
Medical graduates are seeing GPs with a varied career portfolio and.. that looks attractive
Dr Tom Micklewright
This is a route being pursued by NHS England too. Acting director of primary care Dr Nikita Kanani says: ‘As someone who juggles being a GP with my NHS England role and a young family, it’s clear… the NHS needs to continue to embrace a range of working patterns and offer varied career options.’
And medical graduates seem to be heeding this message. Last month Mr Hancock announced 3,473 had signed up for GP training this year – a record number and the first time the 3,250 target has been exceeded – and HEE ascribes this in part to its emphasis on the flexibility of general practice.
Of course, adapting to part-time working will need extra funding for general practice – starting with cash from NHS England’s 10-year plan, set to be announced before the end of the year.
BMA GP Committee chair Dr Vautrey tells Pulse: ‘As more doctors use the flexibility that general practice can offer to develop a working pattern that suits them, we will need to train and recruit more. But by offering better working conditions and a better work-life balance we may be able to retain more GPs as well.’
But he adds: ‘It is vital the Government provides the investment to rectify the recruitment and retention crisis so GPs feel working hours are more manageable, while providing the flexibility and support for those wishing to broaden their scope.’
GPs are changing. With the right support and structures, this part-time revolution could put the profession on a positive path to the future. It is up to the Government and NHS England to ensure there are not too many casualties along the way.
- Additional reporting: Beth Gault

















