Exclusive One in 20 GPs is considering closing their practice within six months, in the latest indication of the drastic action the profession is considering to survive.
A Pulse survey of nearly 600 GPs found 5% were thinking about handing back their contracts to NHS England within six months.
Nearly 13% said they could not see their practices remaining viable beyond the next two years.
The survey reveals the deep uncertainty within general practice, with GPs citing overwork and burnout as reasons for them considering giving up their contracts.
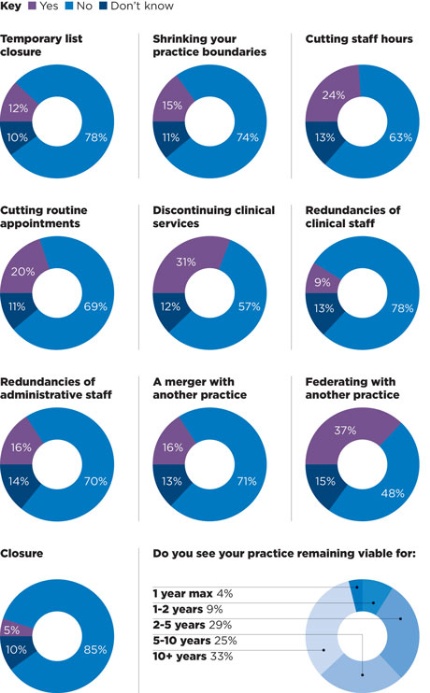
One in ten (12%) said they were considering applying for a temporary list closure, while 15% said they were thinking of shrinking their practice boundaries.
And many GPs admitted to having to make staff cutbacks to stave off closure, with 16% considering redundancies among their admin staff and 13% thinking of making cuts among their clinical staff in the next six months.
GP leaders told Pulse the survey results were ‘sadly, all too common’ and indicated that NHS England’s Five Year Forward View proposal for an emergency package for general practice may come too late for GPs who are at the ‘end of their tether’.
The latest figures come as Pulse continues to campaign for emergency support for struggling practices and major increases in long-term investment as part of its ‘Stop Practice Closures’ campaign.
The RCGP said last month that more than 500 practices in England could close within a year because of a ‘deepening crisis’ in the recruitment and retention of GPs, and a Pulse investigation revealed in July that 100 practices had closed or were facing imminent closure.
The results of the survey of 564 GPs found:
- One in 10 are considering applying for a temporary list closure in the next six months
- 15% are considering shrinking their practice boundaries
- Nearly 4% see their practice viable only for one year max, and 9% for one to two years
- Only one third can see their practices remaining open for 10 years or more
- One in 10 are considering making clinical staff redundancies
- 15% are considering making administrative staff redundant
- 24% are considering cutting staff hours in the next six months
- A fifth of GPs may cut routine appointments
- Nearly a third (30.5%) will consider discontinuing some clinical services
- 15% are considering merging with other practices
Dr David Marr, a GP in Dukinfield, Cheshire, said he would be retiring early from his practice in April 2015, leaving his partner to manage alone and that he expects the practice to close within the year.
He said: ‘[There’s a] lack of enthusiasm for partnerships amongst trainees. The BMA standard contract makes salaried GPs (with all the benefits and no responsibility) too expensive.’
Dr Agnelo Fernandes, a GP partner in Croydon, said that he would be handing his contract back to NHS England due to a ‘serious loss of funding’.
And Southampton GP Dr Alan Mayers said: ‘[It’s] getting harder and harder to meet all the demands, and we can’t recruit. With falling MPIG, running two sites is going to be financially very difficult.’
GPC deputy chair Richard Vautrey said the results showed a reality that was ‘all too common now’. He said: ‘They reflect the growing workload pressures and real stresses that GPs are under. And it’s not a surprise that many GPs have reached the end of their tether and taking very difficult decisions.
‘The NHS Five Year Forward View that was released last week, it was talking about stability of funding in the next two years and increased investment in primary care in the next five years, we need to see that much, much quicker to enable practices to support the core work they’re delivering.’
Are you considering the following within your practice over the next six months?
The survey launched on 7 September 2014, collating responses using the SurveyMonkey tool. The 29 questions asked covered a wide range of GP topics, to avoid selection bias on one issue. The survey was advertised to readers via our website and email newsletter, with a prize drawer for a Samsung HD TV as an incentive to complete the survey. Some 564 GPs answered this question.


















