A diagnostic aid providing early support to GPs during the initial stages of patient consultation improved their diagnostic accuracy, according to a recent study.
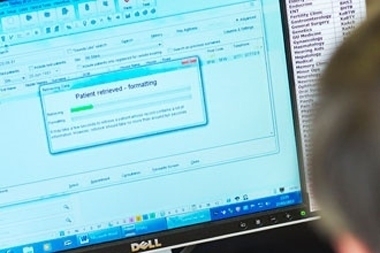
The diagnostic support system (DSS) tool requires GPs to enter an initial reason for the patient seeking a consultation, and then displays a list of possible diagnoses based on the patient’s age and sex.
As more symptoms are added to the tool, the list of diagnoses is reordered based on the amount of information supplied and the diagnostic incidence of each condition.
The study, carried out by researchers at the University of Dundee, found that when 34 GPs used the tool in simulated clinical scenarios, with actors playing patients, there was an 8% absolute increase in diagnostic accuracy to 58%, compared with 50% when they used their own judgement.
The researchers said that while the precise psychological mechanisms through which the DSS works, and its impact on cognition, are not known, it is possible the tool ‘has a debiasing effect by disrupting intuitive thinking based on first impressions, and encourages a more reflective or cautious approach’.
The GPs did not spend longer in consultations or order more tests when using the tool and reported they were satisfied with the tool’s ‘usability’. In addition, patient satisfaction ratings were similar between consultations with and without the DSS, leading the authors to state that they found ‘no evidence’ for the use of such tools affecting the doctor-patient relationship.
The GPs also added significantly more data into the patients’ notes when using the DSS, as the tool’s integration with the electronic health record system allowed information to be coded in real time.
The team concluded that the tool ‘has the potential to be employed successfully, and lead to improved coding, diagnosis, and management, without significant costs in time, tests, and patient satisfaction’.
Br J Gen Pr 2017; available online 30 January