Once again, GPs are set to bear the brunt of a crackdown on referrals that is likely to heap more work onto practices.
This time, NHS England is pushing plans for GPs to peer review all colleagues’ referrals every week in a bid to drive down the costs of secondary care activity.
Managers are funding CCGs to implement the proposal, and Pulse has learned some have got them under way.
But GPs are angry at the plan, calling it ‘flawed’. They also say peer review is unnecessary, after the latest official statistics showed practices are starting to arrest the increase in referral rates.
And some commissioners have already ditched the schemes after finding they have little effect.
The plans for peer review have not been made public by NHS England, but were revealed after Pulse obtained a leaked document in August.
The document – entitled Elective Care High Impact Interventions: Clinical Peer Review – tells commissioners they will be eligible for ‘significant additional funding’ in 2017/18 if they ensure GPs review each other’s new referrals, at least once a week by the end of September.
The document recommends smaller practices work in ‘clusters’ to ‘share learning and increase the specialist knowledge pool’, and that CCGs share monthly referral and secondary care activity reports with practices ‘so they can review trends and compare to peers’.
It suggests ‘CCGs may wish to consider prioritising the top 25% of high referring practices for initial roll-out and additional support’ and claims this could help reduce referrals by 30%.
But the guidance makes clear the system ‘should not be established as an approval process’ and the ‘referring GP retains responsibility for the patient and makes the final decision’.
NHS England was unable to say how many CCGs have received funding for the scheme, but Pulse has seen a leaked internal memo from NHS Bedfordshire CCG that said local leads are insisting all practices are implementing it. A CCG spokesperson says: ‘Details of the agreed system will be advised in due course’.
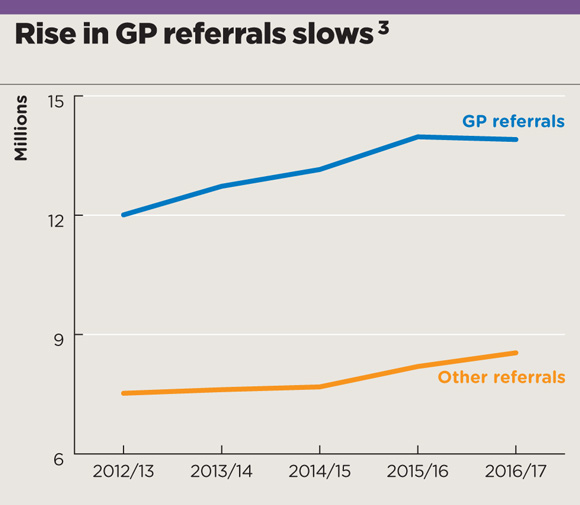
Referrals rise graph Oct 2017 – Large
Referrals rise graph – large
Doncaster LMC medical secretary Dr Dean Eggitt says there is also a peer-review referral management system in place in Sheffield.
Dr Eggitt says such systems have been shown to reduce referrals and costs associated with outpatient appointments, but adds: ‘They undermine the professionalism of colleagues and do not take into account the consequent increased workload undertaken in primary care, the associated demand on primary care resources and the unfair burden of accountability returned to the primary care clinician who has requested specialist support via the route of referral.’
NHS England claims that peer review schemes can reduce referrals by 30%, based on a King’s Fund study. An NHS England spokesperson said: ‘Clinical peer reviews are a simple way for GPs to support each other and help patients get the best care, from the right person, at the right time without having to make unnecessary trips to hospital.
‘More than half of CCGs have already implemented a peer review system, with Luton seeing an 8% drop in hospital referrals, and the latest NHS England guidance will help ensure best practice is shared to local commissioners.’
However, not all have found these schemes work. NHS Basildon & Brentwood CCG ditched its scheme last year. A spokesperson said: ‘The CCG had a peer-review referral management scheme, which was reviewed last November. This showed that while the scheme was in operation referrals from GPs rose by 17%. At an annual cost of £285,000, the CCG decided to end the scheme.’
However, since NHS England released the guidance, the CCG has begun consulting on how it can implement a new peer-review scheme.
They undermine the professionalism of colleagues
Dr Dean Eggitt, Doncaster LMC medical secretary
NHS England has suggested a number of other ways for CCGs to ensure GP referrals are ‘appropriate and necessary’. Its Demand Management Good Practice Guide, published last year, recommends greater use of ‘shared decision making’ processes with patients and better ‘advice and guidance’ for GPs on referrals. This involves ‘breaking down barriers between clinicians in different care settings to raise the quality of referrals and ensures that patients are referred to the right place, first time’.
But while such measures might be helpful, there is little to suggest this help has yet been made widely available to GPs. There is also a sense of resentment among GPs, who say they are beginning to cut referrals despite increases in primary care activity.
NHS England figures published in August show GP referrals decreased by around 0.5% compared with the previous year, at a time when referrals from elsewhere were rising.
GP leaders say this success makes peer review schemes for all practices unnecessary. Indeed, the BMA is calling for NHS England’s plan to be withdrawn.
Its GP Committee chair Dr Richard Vautrey says: ‘We have raised our serious concerns with this flawed peer-review plan proposed by NHS England. At a time of massive pressure on practices, plans that place barriers between GPs and specialists and undermine the professionalism of highly trained GPs are not the way to improve patient services.
‘We are aware many CCGs have also raised concerns. We have called on NHS England to withdraw this document.’
















