GP practices on an industrial scale are starting to evolve in some parts of the country.
Areas used to being served by a number of small practices are now seeing them merge to become mega-partnerships with lists covering hundreds of thousands of patients.
Even the GPC has recently said in its vision for the future that super-practices could be one of the few ways of ensuring the ‘core principles’ of general practice are retained.
List sizes have grown by 28% since 2002, while the number of singlehanders has plummeted. The trend now looks to be accelerating.
Earlier this year, Pulse reported a 500% rise in practices telling NHS managers they wish to merge or close, often due to funding cuts or recruitment problems. And now some practices are now taking their future into their own hands by entering talks to form huge super-practices.
Going large
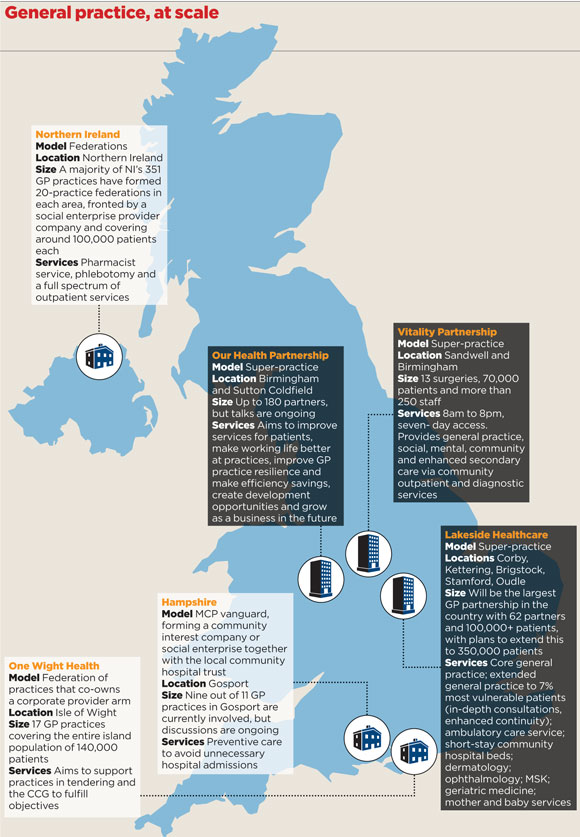
Pulse has learned that next year will see the launch of the largest-ever GP practice in the NHS, with 62 partners, covering over 100,000 patients at Lakeside Healthcare in the East Midlands. Lawyers say this will not be the only super-practice to launch over the next few months, and it is set to be dwarfed by one being formed in Birmingham and Sutton Coldfield.
GP leaders in the region are currently in merger talks, and although precise details are under wraps until the deal is finalised later this year, Pulse understands it could involve as many as 180 partners.
Dr Mark Newbold, managing director of Our Health Partnership, says the move is important for the ‘security, support and sustainability’ of local practices.
He explains: ‘There are recruitment issues at the moment and many smaller practices are not robust. If one or two people retire or leave then that practice is very difficult to sustain.’
Dr Newbold says the super-practice will merge back-office administrative functions, save money through bulk buying and have greater access to locum and holiday cover through a ‘pool’ of GPs for the region. He adds: ‘Practices will be able to stay in the same premises and so services will remain local. This partnership could allow us to provide extra services, such as home care or post-hospital care. We’re effectively moving from the GP model towards an “accountable care organisation” model.’
And this is a direction of travel that is sanctioned at the highest level of the health service. NHS England chief executive Simon Stevens said accountable care organisations are the future, saying it was ‘mission-critical’ to ‘blur the old boundaries between GP and hospital care’.
NHS England is signalling the emergence of even larger GP-led organisations, with the piloting of the ‘new models of care’ in its Five Year Forward View. These ‘vanguard’ projects are tasked with trialling new, more financially efficient models that could be rapidly rolled out elsewhere in the country and help the NHS make the £22bn savings demanded by Mr Stevens by 2020.
Stronger voice
The Lakeside Healthcare practice will be the largest GP practice in the country, under its multispecialty community provider pilot – the GP-led model specified by NHS England. Its chair Dr Peter Wilczynski, a GP in Corby, says the 62-partner practice will focus on providing ‘extended primary care services’ to the most vulnerable 7% of patients, with in-depth consultations and enhanced continuity of care.
Dr Wilczynski says the merger will boost the GP voice: ‘We have chosen a partnership merger model because that leaves us with one voice, one organisational governance framework and one clinical governance framework.
‘A lot of GPs have real difficulty in giving up strategic autonomy, but the reality is that they don’t have it because they are too small to influence decision-makers at a commissioning level.’
And more large-scale mergers look set to follow. Robert Capper, a partner at Harrison Clark Rickerbys solicitors, tells Pulse he has recently advised on two large mergers, which are not yet in the public domain. He says: ‘We regularly advise on practice mergers. Our largest to date has been a seven-practice merger with 50-plus partners. We are currently working on a three-practice merger with 35 partners.’
But Dr Jonathan Ireland, chair of Northamptonshire LMC, which covers the Lakeside Healthcare area, says some patients are unsettled by the idea of such large GP practices.
Dr Ireland says: ‘I know for a fact that some patients don’t like the size of the organisation and have sought out smaller practices to join instead. Lakeside probably does not agree with this, but there is the risk of losing continuity of care with patients. A larger organisation will mean some inevitable fragmentation.’
But it seems there is a belief among GP leaders that this is the least worst option for the future of general practice. The GPC’s vision for the future of general practice, published last week, highlights federations and super-practices, which would form collaborations with other providers of health and care in return for more funding from the NHS, it suggests.
The document says: ‘A collaborative care model… reflects the core principle of GP-led primary healthcare, which doctors and patients want to see retained.’
Family Doctor Association chair Dr Peter Swinyard, arguably the biggest cheerleader for the small family practice, has even considered upscaling.
He tells Pulse: ‘I think this is now a matter of circling the wagons in a very hostile environment to protect practices from the ravages of underinvestment of the Government and the lack of GPs.’
Dr Swinyard believes the new super-practice models ‘will start to be predominant over the next couple of years’, as long as the ‘basic interaction with patients’ remains in place, and they are within a ‘push pram’ of patients’ homes.
He says: ‘Indeed, I have had ideas of trying the same thing in the Swindon area, where we have a good record of practices working together for the common good. We have to reduce overheads and make our practices somewhere where people want to work and where patients are well cared for.
‘Larger groups will have an ability to tender for services that is completely beyond the reach of single practices – I think the future starts here.’
Dr Robert Morley, executive secretary of Birmingham LMC and GPC lead on contracts and regulations, agrees that large partnerships are the only way forward.
He says: ‘Like it or loathe it, the landscape is changing radically and very quickly. The small business model of general practice sadly is no longer capable of surviving in the NHS as it now is, and GPs have to adapt and work at scale.’
What is a super-practice?
A ‘super-practice’ is a single organisation, rather than a federation of practices, and is often formed by a series of list mergers.
The GPC defines it as one GP practice covering a very large patient population, potentially in excess of 100,000. While officially a single practice, a super-practice often operates from a number of different sites within an area, with practice staff working across sites.
It is often run by a small group of partners within the organisation, although it can have a wider partnership base, with a small group elected or appointed from among the partners to take on a managing executive role.
As in federations, the practice may centralise certain functions, such as having a single point of access for telephone contact. In a federation, GP practices retain separate partnership deeds, and often separate clinical governance standards, while collaborating on things like enhanced services.
But the super-practice provides a much stronger management structure than a network of independent practices and can ensure greater consistency of standards across the different practice facilities.
Super-practices can collaborate with other similarly sized NHS organisations within an area but may also compete with them.
They often employ more salaried GPs and a greater range of other community staff than traditional practices.
Source: BMA. Responsive, safe and sustainable: Towards a new future for general practice