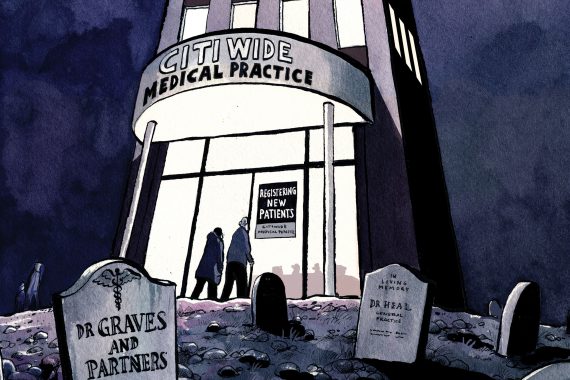
Although federating is currently seen to be the way forward for primary health care in the eyes of many, there is still much resistance when it comes to accepting this model in general practice as shown in the recent Pulse article ‘Is federating putting practices at risk?’ Much of the discussion surrounding GP federations has involved talk of ‘practices worse off than if they had stayed on their own’ and ‘loss of money for practices and partners, and loss of services for patients’, when in fact this is not always the case as we have shown through our research.
Federations may well offer many opportunities for GP practices, particularly those at risk
We evaluated South Cheshire and Vale Royal GP Alliance’s involvement in wave 2 of the Prime Minister’s Challenge Fund (PMCF). They were awarded £1.9 million to increase access to 24 of their 30 GP practices over a one year period.
We carried out interviews with 90 members of staff across the 24 practices involved with the PMCF, including GPs, practice managers, nurses and admin staff. The findings revealed a number of over-arching themes. The data showed that all practices involved in the PMCF had their own ways of running the scheme, based on their patient population and the ability of the practice itself to run additional clinics. Generally, staff had a positive attitude towards the scheme, with one patient experience manager stating: ‘If we didn’t have our extended hours and our PMCF it would be a lot more strain on the core hours, the core staff, and the core equipment – and that is what isn’t sustainable’. There has also been appreciation from GPs in terms of the opportunity to explore a new income stream.
In regards to the impact on staff, the findings suggested that in many cases there are some staff who are, and some staff who are not, willing to take on weekend and evening shifts, with one GP stating, ‘Two of our GPs actually like coming in early and finishing early and they have kids and can spend a bit more time with them in the evenings… My PM says to me do I want to work a Saturday and I say hell no!’ The scheme was also found to impact the running of practices, with practices having issues such as staff shortages and security problems.
However, the PMCF has also had positive implications on practices, with one practice manager stating, ‘And even taking the finance away, the other benefit is that it pulls people together, gets practices working together. And I always like that. Fifteen years ago, I was in secondary care, so I was used to sharing. But then I came into primary and everything was a secret! How bloody daft is that? So, when you get the alliance working together and you put some money with that… I’m all for it!’
This practical example is evidence that working together as part of an alliance or federation can be beneficial to a practice. Working together through the South Cheshire and Vale Royal GP Alliance enabled 24 practices to successfully bid for the PMCF contract, a substantial sum of money. It did not remove practice autonomy as the project was then rolled out in a way that allowed each practice to work the scheme to their own strengths, while fulfilling the needs of their patients. Federations may well offer many opportunities for GP practices, particularly those at risk. A successful federation though is one that also recognises, and responds, to the fundamental need for flexibility at a practice level.
Lauren Sinton is a PhD student, Dr Philippa Hunter-Jones is a reader in marketing and Dr Lynn Sudbury-Riley is a senior lecturer in marketing at the University of Liverpool Management School
Dr Neil Paul is PMCF project lead for the South Cheshire and Vale Royal GP Alliance and Mike Pyrah is PMCF Project Manager