
ampoule of nebido drug suo spl 3×2
Testosterone has historically been a rarely prescribed drug, taken only by the few men suffering from hypogonadism.
But the marketing of the drug has become more sophisticated in recent years, going as far as promising to give men their ‘oomph’ back.
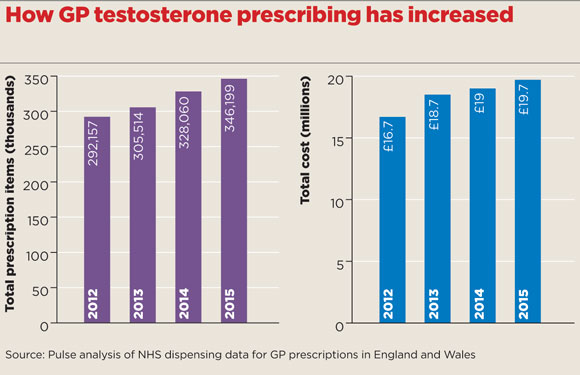
As a result, GP prescribing of testosterone has risen 20% since 2012, costing £20m a year, with both testosterone and testosterone undecanoate entering the top 10 most commonly prescribed controlled drugs in England and Wales.
This continues a shift that has seen prescriptions more than double in primary care over the past decade, and some GPs have expressed concern this ongoing trend could put men at risk.
Recent research contradicts the idea of a natural decline in testosterone with age. The European Male Ageing Study showed the majority of so-called late-onset hypogonadism in men is down to the increased burden of diseases like obesity and diabetes in older age.1 And the treatment is not without risks – for example, poorly monitored testosterone therapy has been linked with complications such as stroke.2
The actual amounts prescribed are relatively modest; around 200,000 items of testosterone and 120,000 of testosterone undecanoate were prescribed in 2015 in England and Wales.
But analysis of NHS data by Pulse shows a steady year-on-year increase, with almost a 20% rise in the overall number of testosterone prescription items dispensed since 2012.
And this follows a large but steady increase documented over the preceding decade; the number of UK testosterone prescriptions shot up 90% between 2001 and 2010, according to one study.3
Male menopause
The total annual cost now stands at £19.7m a year – compared with just £3.2m in 2001.
But GPs are sceptical about how much of the increase in use of testosterone is really justified, particularly in older men.
RCGP prescribing advisor and North Wales GP Dr Martin Duerden says he has concerns testosterone is increasingly being used in the UK to treat ‘the male menopause’ among those with reduced energy and libido, ‘rather like oestrogen has been used in women as an “anti-ageing” product in the past’.
Critics have cited the example of the US, where direct-to-patient advertising and the private health system are widely credited for a ten-fold rise in testosterone use between 2001 and 2011.4
Although there is no direct-to-patient advertising in the UK, some believe the pharma industry is still able to exert influence, putting GPs in a tricky position.
Experts from the University of Newcastle highlighted a possible link between increased marketing in the medical media of testosterone replacement therapy and a sudden increase in prescriptions, despite the absence of clear efficacy data for the treatment.3
testosterone prescribing box 580x375px
Media influence
The team, led by Professor Simon Pearce, reported that ‘a plausible explanation for the observed trend in testosterone prescribing in the UK is that an increasing number of eugonadal men might be receiving unnecessary testosterone therapy, particularly older men with “non-gonadal” illness’, and that ‘pharma has promoted testosterone therapy to a broader population of older men with sexual dysfunction’.
They said that while direct-to-consumer marketing is not permitted, ‘the public has virtually unfettered access to pharma websites as key sources of information relating to ageing, erectile dysfunction and the “andropause”’.
GPC prescribing spokesperson and East Yorkshire GP Dr Andrew Green agrees. He says: ‘Patients with non-specific symptoms or indeed just the normal changes in sexual function that happen with age are influenced by articles in magazines and request testing, which can then result in expectation to prescribe for low-normal readings.’
The rise shows GPs responding to guidelines
Professor Mike Kirby
Testing in private clinics is also piling the pressure on GPs, Dr Green adds.
‘If private clinics test for this as part of their services, the expectation to prescribe is then passed to the GP,’ he says.
But other GP experts argue the rise is being driven by GPs getting better at identifying and treating hypogonadism in men with low sexual drive, erectile dysfunction and decreased energy levels.
Professor Mike Kirby, GP and visiting professor to the Prostate Centre, London, says the rise shows GPs responding to greater awareness of the problem, and to guidelines promoting testing and treatment of hypogonadism in men presenting with erectile dysfunction, such as those from the British Society of Sexual Medicine (BSSM).5
Professor Kirby says: ‘Since the introduction of Viagra, and more interest in erectile problems, more men are being tested for testosterone deficiency – that’s been a major driver of it.’ He says he believes ‘most of the prescribing is appropriate’ in the UK.
But the problem for GPs is there remains considerable uncertainty about how to diagnose secondary hypogonadism and when low testosterone should be treated, even among endocrinology experts.
The UK Society for Endocrinology has warned of a lack of long-term evidence that assesses the risks and benefits in older men with declining testosterone.6
In a position statement on male hypogonadism and ageing, the society said: ‘Although testosterone replacement therapy has been used effectively for many years in younger patients with classical hypogonadism without major adverse effects, this experience and the risk-benefit balance cannot be extrapolated to late-onset hypogonadism’.
And the definition of ‘normal’ testosterone levels also varies to some extent. The BSSM guidelines on erectile dysfunction recommend GPs should always screen for low testosterone levels, offering a six-month trial of testosterone replacement therapy in men with levels consistently below 12 nmol/L.
However, critics argue for a more circumspect approach, with initial checks for opiate-induced hypogonadism or other drug-related causes, priority given to tackling factors like obesity, and trials of PDE5 inhibitors before testosterone.7
Dr Duerden says: ‘I think we should use these products very cautiously unless there are clear clinical explanations for hypogonadism other than age.’
Expert view: Prescribing testosterone wisely

Dr Martin Duerden – online
A large part of the growth in testosterone prescribing is thought to be for older men with waning levels of testosterone, complaining of low sex drive and general loss of energy – the so-called ‘andropause’ or late-onset hypogonadism (LOH).
But LOH symptoms are non-specific, such as: fatigue; reduced physical endurance; mood disturbance; and loss or reduction in libido and morning erections. There are also concerns testosterone therapy might increase cardiovascular and prostate disease risks. To avoid ‘overdiagnosis’ of LOH and overuse of testosterone, keep the following in mind:
- Treatment should ideally be initiated by an endocrinologist, with GPs providing repeat prescriptions. Some CCGs have agreed ‘shared care guidance’ to facilitate this.
- Testosterone levels should be measured twice, at least a week apart, and blood should be taken before 11am.
- Patients need careful examination for cardiovascular disease (including blood pressure) and prostate disease before therapy. This needs repeating at regular intervals (every six months or so) while on treatment.
- Measure blood testosterone after two to four weeks to see if testosterone levels have normalised and check adherence.
- Be vigilant. Some websites will sell prescriptions of testosterone products following ‘online consultation’ with a doctor (not necessarily a specialist or endocrinologist). GPs may not be informed about these prescriptions, so consider this source when consulting with patients.
Dr Martin Duerden is clinical senior lecturer in health economics and medicines evaluation at Bangor University and a GP in North Wales
References
1 Rastrelli, G et al. Development of and recovery from secondary hypogonadism in aging men: Prospective results from the European Male Ageing Study. J Clin Endocrinol Metab. Online May 2015. tinyurl.com/za6vlsp
2 Basaria, S et al. Adverse events associated with testosterone administration. NEJM 2010; 363: 109-122. tinyurl.com/h8e9dxe
3 Gan, E et al. A UK epidemic of testosterone prescribing, 2001-2010. Clin Endocrinol. 2013; 79:564-570. tinyurl.com/jd72rfo
4 Handelsman, D. Global trends in testosterone prescribing, 2000–2011: expanding the spectrum of prescription drug misuse. Med J Aust 2013; 199: 548-551
tinyurl.com/mnpt8yo
5 British Society of Sexual Medicine – Guidelines on the management of erectile dysfunction.
tinyurl.com/gofqttx
6 Society for Endocrinology – Position statement on male hypogonadism and ageing. tinyurl.com/h9pnjnn
7 Endocrine Society of Australia. Position statement on male hypogonadism (part 1): assessment and indications for testosterone therapy. Med J Aust 2016; 205: 173-178. tinyurl.com/jx3kyvy

















