Picking up on our series of scenarios that are commonly mishandled in primary care, Dr Peter Bagshaw looks at how to avoid being misled by an incidental finding of gallstones
The scenario
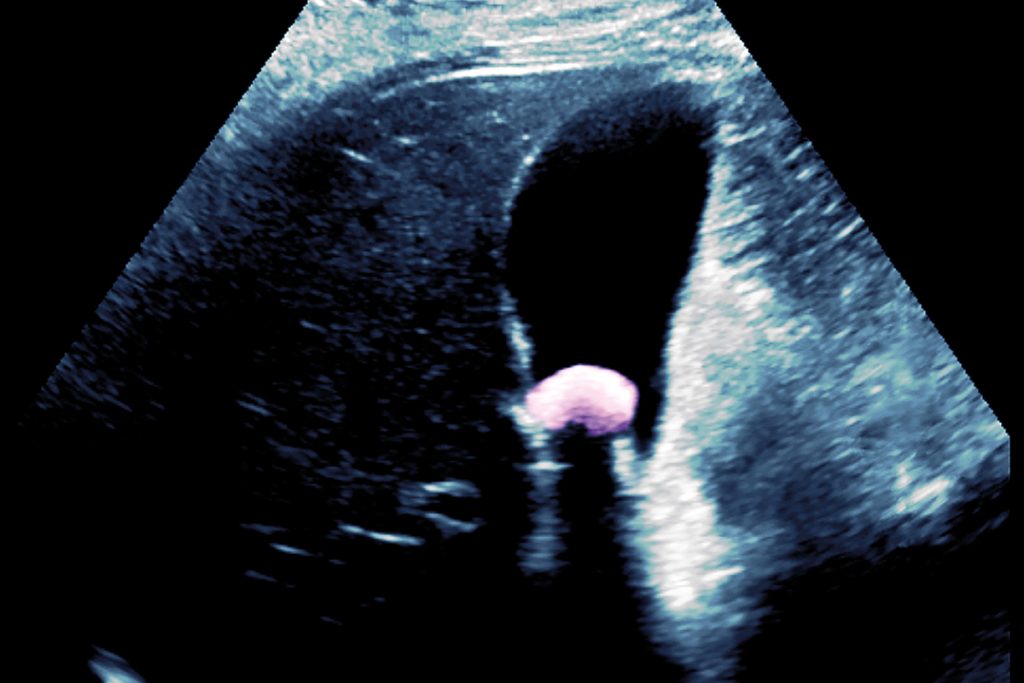
A 42-year-old man presents with vague upper abdominal pain. He describes it as ‘crampy’ and intermittent. There is no weight loss, change of bowel habit or gastrointestinal red-flag symptom, and no clear relationship to food or posture. Examination is normal with no tenderness or masses; screening bloods are all normal, but an upper abdominal ultrasound reveals the presence of gallstones. The patient is keen to be referred for surgery to solve his problem.
The reality
Asymptomatic gallstones are a common incidental finding and do not require treatment. If the abdominal pain is not typical biliary colic, it is unlikely to be due to gallstones even when these are shown on ultrasound.
Abdominal pain may be due to a number of possible causes; I was taught 32 but the Mayo clinic lists 63.1 Often it is intermittent and with minimal signs, making diagnosis difficult. While the site and nature of the pain, and the age and gender of the patient can be helpful in pointing us in the right direction, it is often difficult to be sure what the cause of the pain is. In such cases, assuming no red-flag symptoms, screening bloods and an abdominal ultrasound are a reasonable way of proceeding. If the scan shows gallstones, how likely is it that we have identified the patient’s problem?
The classic presentation of gallstones (epigastric or right hypochondrial pain occurring an hour or so after a fatty meal and abnormal liver function tests) can make biliary colic easy to spot. Around 60% of patients suffer recurrent pain within two years, and the potential complications of cholecystitis, cholangitis or pancreatitis mean that such patients should be referred for cholecystectomy.2 However, things will often be more complicated. The pain can sometimes be left sided, central, felt in the back or elsewhere. Small bowel obstruction due to gallstone ileus can be the presenting feature, and atypical symptoms are not unusual and include chest pain, belching, rapid satiety, dyspepsia and non-specific abdominal pain.3 Half of those with gallstones will have no symptoms, and they do not need referral as complications are unlikely.4
The evidence
A study of patients undergoing diagnostic ultrasound for conditions other than gallbladder disease found that 5% of women aged 30-39 had asymptomatic gallstones, as did 11-14% of men and women over 40. Despite the famous ‘five Fs’, slightly more men than women had gallstones over 40, and obesity was a factor in women but not men.5 NICE reviewed the evidence for referring asymptomatic gallstones and concluded that for most people in this group the risks of treatment outweighed the benefits.4 When abdominal pain is non-specific, as it so often is, gallstones should be considered, but alternative diagnoses such as peptic ulcer disease, hiatus hernia, gastro-oesophageal reflux disease, irritable bowel syndrome (IBS) or dyspepsia are more likely. 6 Even in those felt to have biliary colic, pain is only relieved in 82% of those having a cholecystectomy, implying that some have pain from another cause.7
Avoiding a clanger
The incidental finding of abnormalities on increasingly sophisticated imaging can pose a major dilemma for GPs. As asymptomatic gallstones are common, particularly in older people, it would be unwise to assume they are the cause of the patient’s symptoms unless the clinical presentation is fairly typical for biliary colic. IBS, peptic or oesophageal disease should still be considered, as should non-abdominal pathology such as cardiac disease or pneumonia. Abdominal pain in primary care remains challenging.
Key points
- Only diagnose ultrasound-revealed gallstones as the cause of abdominal pain if the symptoms fit with biliary colic
- Asymptomatic gallstones are common, becoming increasingly so with age
- In over-40s they are as common in men as in women
- Complications are rare, and asymptomatic gallstones can be managed by watchful waiting
- Red flag two-week-wait gastrointestinal symptoms should be referred irrespective of the presence of gallstones
Dr Peter Bagshaw is a GP in Somerset
References
- Mayo Clinic. Abdominal pain: Causes
- Callery M et al. In Jarnagin W (editor) Blumgart’s Surgery of the Liver, Biliary Tract and Pancreas (Sixth Edition). Elsevier, 2017
- Biliary colic and complications from gallstones. Best Practice Journal 2014;61: 28-31
- NICE CKS. Scenario: Management of people with asymptomatic gallstones 2019
- Hopper K et al. The prevalence of asymptomatic gallstones in the general population. Invest Radiol 1991;26:939-45
- Wallander M et al. Unspecified abdominal pain in primary care: the role of gastrointestinal morbidity. Intl J Clin Pract 2007;61:1663-70
- Fenster L et al. What symptoms does cholecystectomy cure? Insights from an outcomes measurement project and review of the literature. Am J Surg 1995;169:533-8
















