Consultant nephrologist Dr Colin Jones advises on the diagnosis and management of autosomal dominant polycystic kidney disease in general practice
Learning Objectives
- Know the main form of polycystic kidney disease (PKD) and how it is diagnosed
- Be aware of the role of genetic testing for PKD and how to approach this
- Recognise complications of PKD that may present in primary care
- Know when to investigate for PKD in patients with impaired renal function
- Understand the prognosis for patients with PKD
1. How common is polycystic kidney disease (PKD) and what causes it? What are the genetics of PKD?
The main form of PKD is autosomal dominant PKD, an inherited condition that is relatively common and affects approximately one in 1,000 people. There are two main forms of this condition, involving different gene mutations known as PKD 1 and PKD2.
In general, PKD 1 has a more severe phenotype than PKD 2 and is more likely to cause end stage kidney disease (ESKD) and at a younger age (median age 54 versus 74 years). However, it is important to remember that up to half of individuals with autosomal dominant PKD will not be affected by the ‘disease’ in their lifetime.
There is also an autosomal recessive form of PKD (ARPKD) that is much less common. This form predominantly affects children, often causing serious problems in childhood, although less severe cases may present in young adults. The phenotype (disease manifestations) is different and these children are managed by a paediatric renal physician. It is therefore not dealt with in this article.
Throughout this article PKD refers to autosomal dominant disease (usually referred to as ADPKD).
2. How is PKD definitively diagnosed?
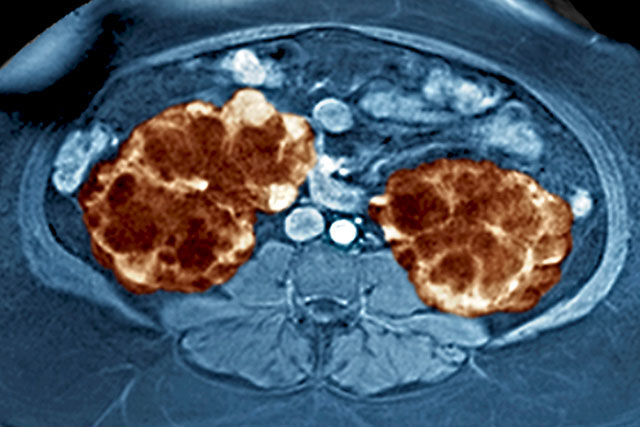
PKD may be asymptomatic and diagnosed in individuals with a family history through screening, either by genetic testing or more usually with renal imaging.
The guidelines for diagnosis based on renal imaging in people with a family history of PKD are complex, but ultrasound is the preferred imaging modality for diagnosis. As a rule of thumb, the absence of any renal cysts on a high-quality ultrasound in someone over the age of 18 years has a high exclusion value. However, this is dependent on genotype and actual age.
Conversely, the presence of cysts in someone with a family history has a high positive predictive value for a diagnosis of PKD, but again this depends on genotype, age and the number of cysts in each kidney and both kidneys combined. For someone without a family history of PKD, the finding of 10 or more cysts in each kidney and kidney enlargement or the presence of cysts in the liver make a diagnosis of PKD more likely.
Genetic testing is usually reserved for more complex situations, where uncertainty over the diagnosis persists. Remember, isolated renal cysts are seen very frequently on renal imaging and many older people have more than one simple cyst.
Click here to read the full article and download your certificate logging 2 CPD hours towards revalidation
Dr Colin Jones is a consultant nephrologist at York and Scarborough Teaching Hospitals NHS Foundation Trust
Not a Pulse365 member? Click here to join and gain access to over 400 CPD modules
















