So what about this new app they’re developing? You know, the one the politicians are promising? Apparently, and I think I’ve got this right, it will enable us to book an appointment more easily with Jeremy Hunt?
Which is great, because I’ve been wanting to speak to him about, well, everything. I’ve tried writing, emailing, faxing, Skyping. Nothing. I even joined the ‘Let’s try to get an appointment with Jeremy Hunt’ scramble by phoning him at 8am but of course the line’s always engaged or never answered.
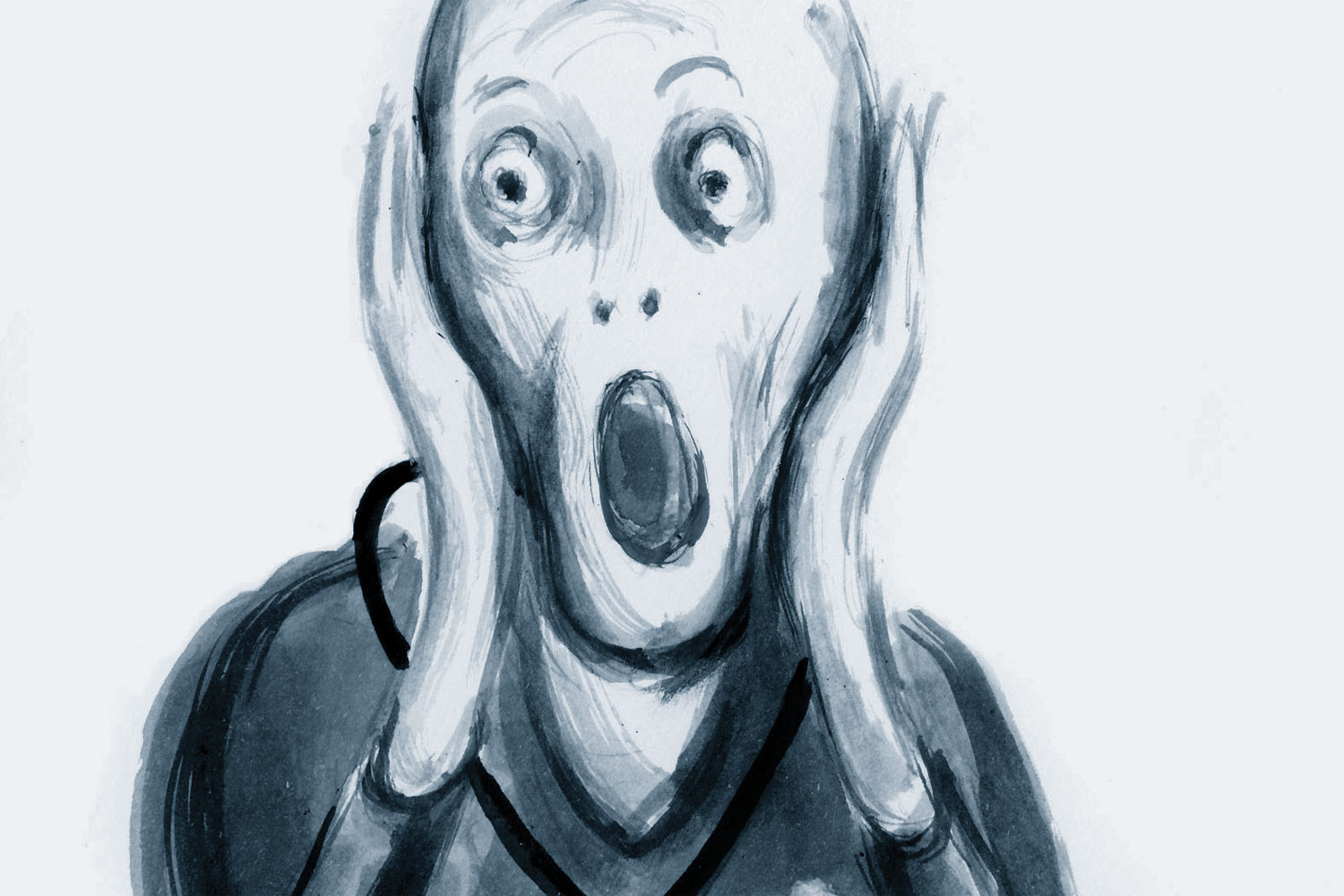
In the end, I tried shouting. I stood outside an important looking door at NHS England yelling until I was hoarse, blue and venously distended, ‘Jeremy, are you there, because I’ve got one or two things I want to shout at you, in particular about how planning to introduce gimmicky technology to access GP appointments is flawed on account of there being no appointments to access.’
Eventually someone opened the door. When I explained how I’d tried to contact Jeremy Hunt via fax, letter, email, Skype, phone and was now resorting to shouting to exercise my right to access a politician, it was explained to me that it’s not that simple. Apparently, there are not enough Jeremy Hunts available to satisfy demand, although NHS England is confident that there will be 5,000 more Jeremy Hunts by 2020.
As a consolation, they did allow me to beta test the new ‘Access a Politician’ app and guess what? I did eventually get to see Jeremy Hunt. But he said I was wasting my, and his, time, because I should have been signposted elsewhere, and that signposting will therefore be incorporated in the app software at some point in the never future.
This made me shout again and he suggested that, for my ‘complex needs’, I should make an appointment with my GP. If only there was an app for that.
Dr Tony Copperfield is a jobbing GP in Essex
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens














