My working life: Specialising in mental healthcare

Profile
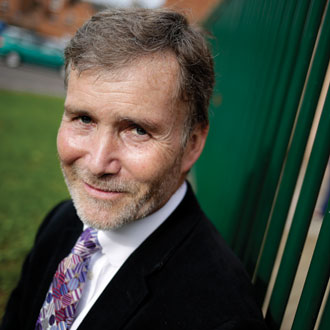
Dr David Smart
Age 53
Role Mental health GPSI and mental health lead at NHS Nene CCG
Location Northampton
Hours a week Around 40 hours in practice, including 12 to 16 hours on mental health work
06.15
The alarm goes off and I go downstairs to make a cup of tea for my wife – always an essential part of my day. For breakfast I have porridge – I’m an addict after reading the research about its benefits for cardiac disease.
07.00
I leave the house and get into work at 8.30. Before surgery I do some admin or catch-up from my consultations the previous day. Mental health consultations take longer than normal consultations, so I often find myself catching up the next day. Because of my special interest, I probably get more than my fair share of these in the practice, especially the complex patients, but I am first and foremost a GP. I don’t have a mental health clinic in the practice – I want everyone to be doing it.
In my consultations, I often just let people talk. At the beginning, I listen for patients’ strengths – I’ve moved away from using diagnostic criteria to trying to find out how patients are coping with their symptoms. That way, I can build their strengths into a management plan with them.
Conversations that focus on what’s wrong can make patients distraught and hard to manage, so strengths-based consulting has helped me find an alternative to ‘deficit’ consulting.
I learned a technique called the 10-minute hour using the acronym BATHE – listen to the background, note the patient’s affect, ask what’s troubling them the most, what’s helping them cope, end with empathy.
I also look for ways in which I might be able to work as a team with the patient, relatives and carers, using resources in the community to give them a sense of hope.
14.00
This afternoon I spend time preparing materials for a tutorial on antidepressants with GP registrars – when to stop and when to switch.
I plan to discuss British Association for Pharmacology guidelines with the students, alongside locality guidelines on prescribing.
To prepare to teach takes around half an hour, as I need to find the resources to facilitate a discussion (which I prefer to didactic teaching).
17.00
I get home after spending the final hour and a half of my working day doing emails as part of my CCG role.
We’re now developing an integrated wellbeing service for the area in partnership with the public health department.
The service combines smoking cessation with weight management and exercise advice. It is funded through a combination of Making Every Contact Count money and various other small grants, and will mainly be delivered through peer support and third sector services, with some help from health service colleagues.
Locally we have a really enlightened director for public health, who promotes wellbeing in the county. The opportunity to link up exercise, libraries, adult education and the third sector is beneficial.
In the evenings, I sometimes prepare for events – for example, a conference I have coming up on GPs’ own mental health. The climate in general practice is the worst I’ve known in 25 years.
GPs need resilience in the same way patients do – you can focus on the negative and the threat, but it just winds you up. But if we focus on the positive, at least we know we are the most trusted profession.
Good consultations can really make a difference to GPs and patients. And the great joy of general practice, particularly when it comes to mental healthcare, is that we can make a great difference to a lot of people – and we don’t have to do anything complicated.
Personally, I keep positive images on my phone and on my desk – for me, these are pictures of my daughters in the local bluebell wood.
A book I recommend to everybody – GP or patient – is Mindfulness: finding peace in a frantic world by Mark Williams. It’s an eight-week course and I recommend them to read a chapter a week. A lot of people have found that helpful.
19.00
I always have supper with my wife. Our two daughters are now at university so we eat with them if they’re around. I exercise about four times a week or go out with friends. But on a quiet night, I head to bed at 23.00.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.










