Exclusive Long waits between therapy sessions may be prompting patients with mental health problems to quit their treatment, leaving GPs to pick up the slack.
Some 42% of patients starting the Improving Access to Psychological Therapies (IAPT) programme only ever complete one treatment session, according to data analysis by Pulse as part of an investigation.
At the same time, and contrary to NICE guidelines, more than half now have to wait longer than a month between their first and second appointment.
Experts and GPs suggested the issue may stem from the introduction of waiting time targets by NHS England, which mean CCGs rush initial appointments but are not incentivised to provide timely follow-ups.
In April 2015, NHS England brought in the target for 75% of people to start treatment within six weeks of referral, and 95% within 18 weeks – both of which are being met at a national level.
GPs have warned patients leaving treatment and waiting between sessions often means the clinical risk of patients is ‘conveniently being dumped’ on primary care.
NHS Digital’s data on why referrals end do not include a specific breakdown showing the reasons why treatment stops, so these figures are likely to be attributable at least in part to patients choosing to drop out or being referred to another service deemed more appropriate than IAPT.
But Pulse’s analysis of the latest NHS Digital data, shows both the proportion of patients leaving treatment earlier and also those waiting over a month between sessions is increasing.
In July 2018:
- 37,051 patients (42%) did not continue beyond one treatment appointment;
- 26,254 patients (50.3%) waited over 28 days between their first and second treatment.
In April 2015, when the IAPT targets were introduced:
- 23,204 people (34%) stopped therapy after one treatment session;
- In July 2015, the first month with comparable data, 18,836 patients (36.5%) waited more than 28 days between their first and second session.
Delays between appointments go against NICE’s guidance on cognitive behavioural therapy (CBT) for common mental health problems, which states treatment for people with depression should consist of ’16 to 20 sessions over three to four months’, while for people with generalised anxiety disorder ‘it should usually consist of 12 to 15 weekly sessions’.
West Kent LMC representative Dr Zishan Syed, a GP in Maidstone, said the pressure to meet initial waiting time targets ‘seems to have a knock-on impact on waiting times for the following appointments’.
‘What we are seeing is a tickbox approach used to give the impression of progress when in fact nothing worthwhile is achieved for patients.
‘By the time a patient is seen at the second appointment, any value from the first will have been lost. These are very worrying times.’
He added: ‘In some cases patients are effectively being discharged with no option but to be seen by the GP, despite extremely high level needs for which we’re not resourced.
‘It often feels that the risk associated with mental health care is conveniently being dumped onto GPs to manage.’
BMA GP committee chair Dr Richard Vautrey said: ‘Commissioners need to be vigilant that people don’t fall through the cracks between different services when their referral isn’t accepted or patients don’t complete treatment.
He added: ‘It’s vital GPs are informed of a patients’ progress to ensure people are getting the follow up they require, and aren’t being put off seeking help or deteriorate further.’
An NHS England spokesperson said: ‘IAPT is widely-recognised as the most ambitious programme of talking therapies in the world.
‘In the past year alone has had over one million people referred for care, met every performance target consistently and most importantly has helped hundreds of thousands of people to overcome their depression and anxiety, and better manage their mental health.’
They added that the NHS ‘continues to support the expansion of the mental health service workforce, including delivering 3,000 more therapists in primary care’.
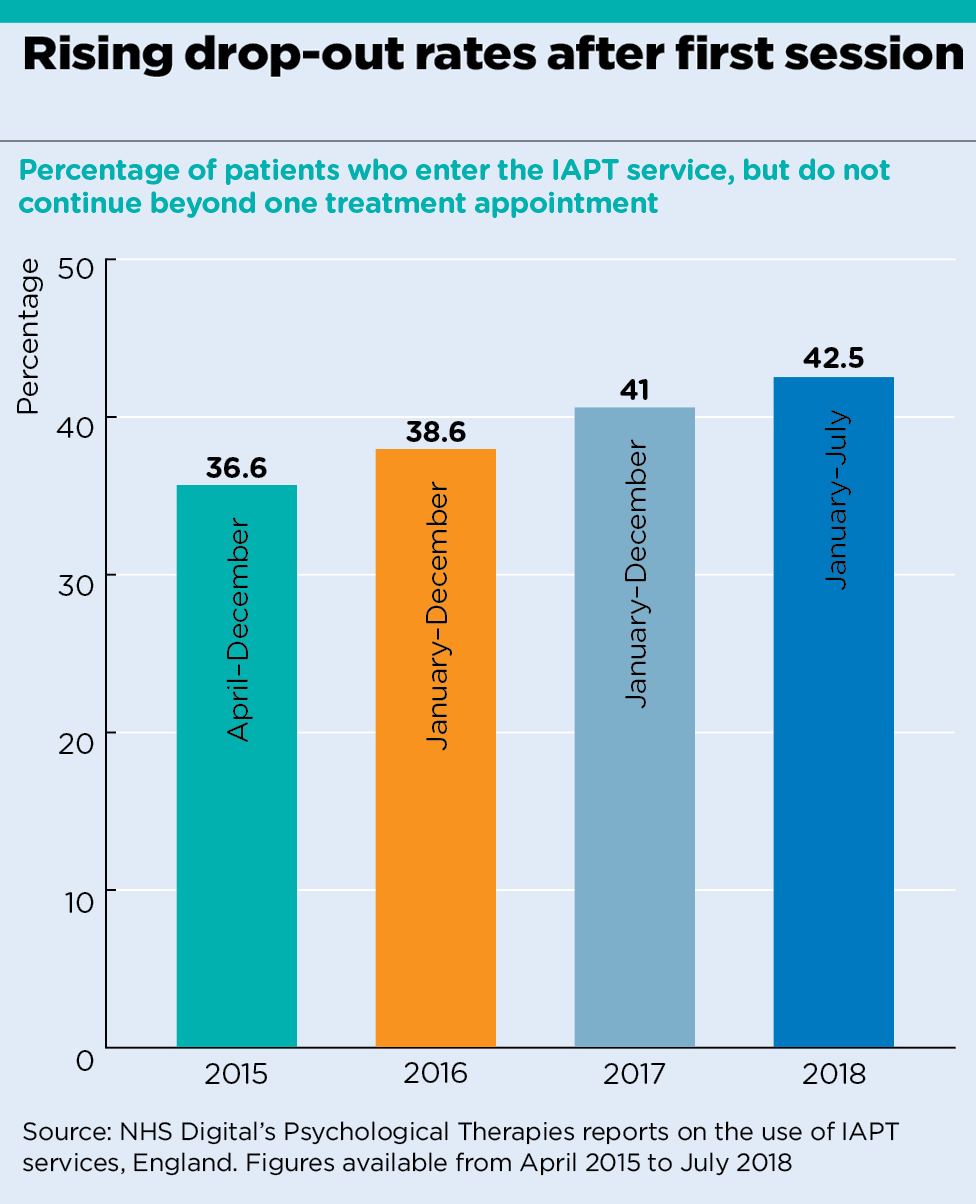
analysis graph 1
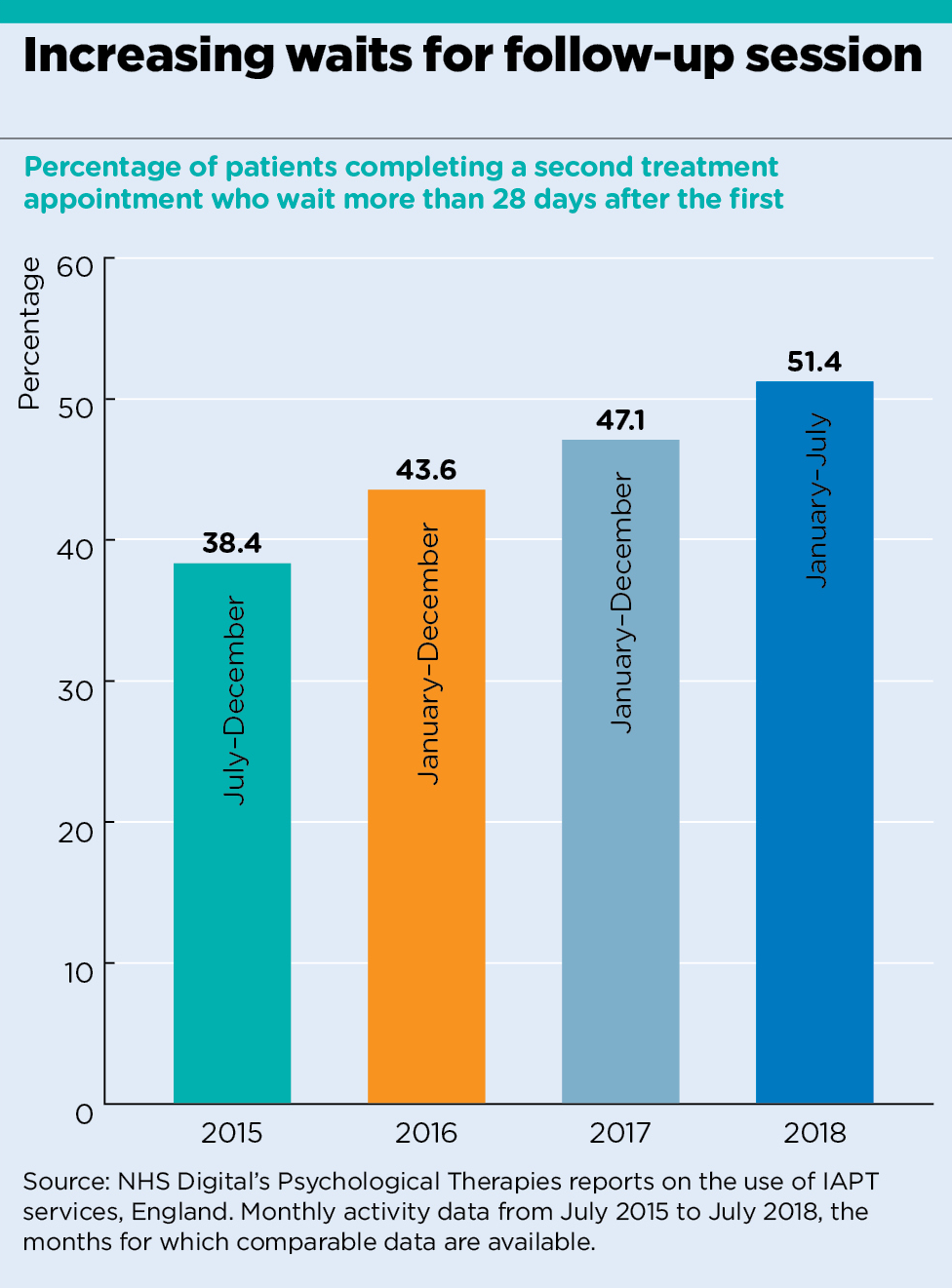
analysis graph 2
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.











