GPs having to deal with angry patients when refusing antibiotics
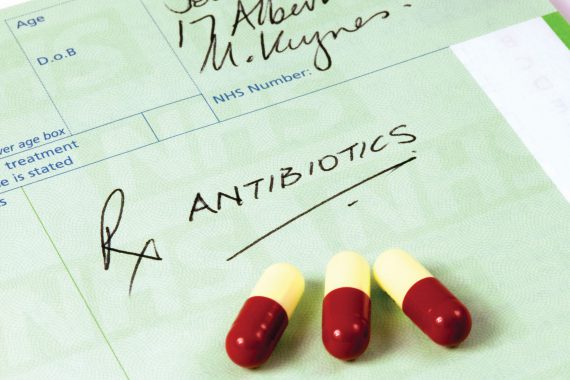
Patients continue to show frustration when they are denied antibiotics, a Medical Protection Society (MPS) survey of 500 GPs has found.
Almost a third (32%) of GPs said that they frequently deal with patients who get angry or frustrated when they are instructed not to take antibiotics.
It comes after Public Health England (PHE) launched a campaign to raise awareness about the higher risks of infections patients could suffer if taking antibiotics inappropriately last October.
Around 5,000 deaths are caused in England due to antibiotic resistance and some studies predict that, in 30 years, resistance will kill more people than cancer and diabetes combined.
As part of the TV and social media advertising campaign PHE made leaflets and posters available for use at GP surgeries, to aid conversations with patients.
About 70% of respondents said they found the campaign useful.
An anonymous GP said: ‘Please carry on with these campaigns as we cannot do it without backup. It is easier to deflect requests if there is information out there.’
However, the MPS survey showed that three in five (60%) GPs decided to prescribe antibiotics to patients when they get angry or frustrated, to avoid confrontation or a complaint, with 4% of them saying they frequently recur to this measure.
Another anonymous GP said: ‘Even when I have prescribed the antibiotics due to the expectation and the frustration of the patient, I do warn them that the antibiotics might not work and give them the reasons why I feel that the antibiotics might not work.’
Senior medicolegal adviser at MPS Dr Marika Davies said: ‘It is understandable that some GPs feel pressurised into prescribing against their better judgment, but GPs should feel confident to refuse to prescribe in these situations.’
‘Prescribing when it is not considered appropriate is not in the best interests of the patient and could put a GP at risk of criticism.’
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.











