Standard current treatment
Smoking cessation
Smoking and passive smoke exposure are associated with worse asthma control and increased exacerbations.1,2 Smoking has also been shown to reduce the efficacy of inhaled steroids.3 Patients and parents should be informed of these risks, advised to stop smoking and offered help to do so.4
Smoking cessation has been shown to improve asthma-related quality of life and reduce drug requirements in adult asthmatics.5 In children with asthma, parental smoking cessation can result in reduced asthma severity.6
Principles of drug management
Standard pharmacological management is described in the British Thoracic Society/Scottish Intercollegiate Guidelines Network (BTS/SIGN) guideline (see figure 1).4 A short-acting ß-agonist reliever inhaler should always be prescribed. The initial preventive regimen should be selected based on a clinical assessment of disease severity, aiming to achieve early symptom control. Subsequently, control should be regularly assessed and treatment adjusted, aiming for the lowest intervention that achieves control.
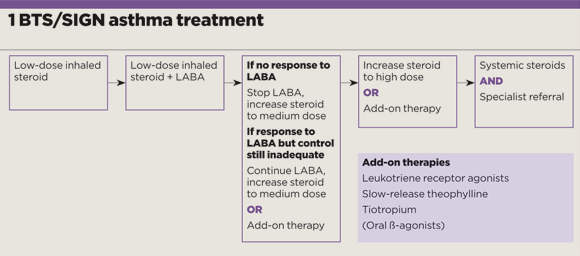
Figure 1
Personalised asthma action plans
The BTS/SIGN guideline advocates offering self-management education and a written personalised asthma action plan (PAAP) to all patients and, if relevant, their parents and carers.4 This is reinforced by NICE.7
PAAPs empower patients to recognise deterioration of their asthma control and escalate their treatment in a timely fashion. Worsening may be identified using a combination of symptoms and peak flows – although for children, symptom-based PAAPs are usually recommended.4 PAAPs improve asthma symptoms and quality of life8,9 as well as reducing sick days9,10 and emergency healthcare utilisation.9,10,11
Inhaler technique
Technique for all devices is notoriously variable among patients and healthcare professionals. One study of 108 patients with obstructive lung disease observed that more than 40% had incorrect technique. However, this figure decreased to fewer than 10% after one training session to correct errors.12
Before prescribing an inhaler, give the patient appropriate training and ask them to demonstrate effective technique.4,7 This is increasingly important as the number of devices available continues to rise. The BTS/SIGN guidance advises against prescribing generic inhaled medications, in case the patient receives an unfamiliar device.4
Treatment adherence
Adherence to treatment for all long-term conditions, including asthma, is approximately 50%.13,14 The reasons for non-adherence are numerous and can include drug side-effects, as well as ideological, financial, social and practical considerations. Adherence should be assessed at each review, and before any therapy is escalated.4 Questions should be specific and non-judgmental, for example: ‘In the past week, how many times have you taken your preventer inhaler?’4 Other sources of data include computerised prescription records, dose-counter inhalers and serum drug levels.
What’s newly available?
Maintenance and reliever therapy
Combination inhalers containing long-acting ß-agonists (LABAs) and steroids are frequently prescribed as maintenance therapy. Maintenance and relief therapy (MART) regimens have been developed that advocate combination inhalers for both prevention and relief. Such regimens involve twice- daily maintenance dosing, supplemented by as-required doses taken when symptoms dictate. A short-acting ß-agonist reliever inhaler is therefore not required in MART.
MART regimens have been shown to result in a lower average daily dose of inhaled steroid, and a reduced frequency of asthma exacerbations requiring oral steroid.15 A MART regimen may be considered for patients over 18 years old who have suboptimal control despite maintenance treatment of medium-dose inhaled steroid or LABA with inhaled steroid.4
In November 2017, NICE issued asthma guidelines that advocate the addition of a leukotriene receptor antagonist (LTRA), such as montelukast, to the regimen of patients with suboptimal asthma control despite regular low-dose inhaled steroid, rather than initiating an inhaled steroid and LABA combination inhaler.
Newer inhalers
The repertoire of inhalers has grown dramatically over the past five years. For example, Relvar is a dry powder inhaler, containing fluticasone furoate (a steroid) and vilanterol (a LABA) and is taken once daily. It is important to recognise that 100µg of fluticasone furoate is equivalent to 250µg of fluticasone proprionate.16
Combination inhalers containing LABA and small-particle steroid have become available. Some respiratory specialists advocate small-particle steroids17 as there is evidence to suggest they are distributed through the whole bronchial tree, including the small airways.18 However, there is a lack of strong trial evidence that this translates to better outcomes.19 Prescribers should note the different potencies of small-particle steroids compared with standard-sized particles. More advanced inhaler devices include the Nexthaler, for formoterol and small-particle beclomethasone, which releases the dose only if the inspiratory flow will result in complete aerosolisation. This has been shown to result in turbulent flow, thought to aid separation of the drug from its carrier molecules.20
Tiotropium as add-on therapy
Devices containing the long-acting muscarinic antagonist tiotropium as an add-on for patients taking inhaled steroid plus LABA are available. A review concluded the addition of tiotropium to steroids and a LABA could result in improved lung function and fewer exacerbations – although no improvement in quality of life was demonstrated.21
What has fallen out of fashion
Subcutaneous terbutaline
Small early studies assessing the efficacy of continuous subcutaneous terbutaline infusion in severe asthma suggested modest improvements.22,23 However, such infusions are associated with a significant side-effect profile and benefits have never been proven in RCTs. As such, their use is not recommended.4
Steroid-sparing drugs
Patients with severe asthma are at risk of side-effects from repeated or long-term steroid use. For this reason, steroid-sparing drugs such as cyclosporin and methotrexate have been trialled. Although such agents have been shown to have a modest steroid-sparing effect, they have significant side-effect profiles and their use is not recommended outside specialist centres.24,25
Atypical cases and their treatment
Severe asthma management
All patients who remain symptomatic despite maximal standard therapy should be seen by a specialist difficult asthma multidisciplinary team.7 This is associated with improved quality of life, reduced symptoms and lower oral steroid requirements.26
Occupational asthma
Occupational factors account for at least 15% of adult-onset asthma.27 A new diagnosis in an adult should prompt an assessment for an occupational trigger.7 At-risk workers include: bakers, laboratory technicians, storage workers, waiters and cleaners. High-risk industries include chemical, rubber and plastic, metal, electrical, food production, textile and forestry.28 A key screening question is ‘are you better on days away from work?’4 Suspicion of occupational asthma should prompt referral to a respiratory physician with expertise in occupational lung disease.29
Asthma in pregnancy
During pregnancy, approximately a third of asthmatic women will experience worse symptoms, a third will remain the same and the remainder will improve.30 Asthma exacerbation in pregnancy is associated with a higher incidence of low birth weight,31 but well-controlled asthma does not confer additional risk to pregnancies.32 Although RCT evidence of the safety of asthma medications in pregnant women is lacking, retrospective analysis is reassuring33 and clinicians should advise women to continue medications during pregnancy to reduce risk to themselves and their baby.4
Non-drug options
Allergen avoidance
Up to 50% of asthmatics are sensitised to house dustmites.34 Consequently, several physical and chemical methods of minimising dustmite exposure have been trialled, including mattress covers, intensive cleaning regimes and acaricides. However, a Cochrane review identified no significant benefit associated with any such techniques.35 There is little compelling evidence that avoidance of any aeroallergens results in significant improvements.35
Exercise and weight loss
Obesity is a risk factor for asthma36, and obese patients have more severe symptoms.37 A Cochrane review of weight-loss interventions for overweight and obese patients with asthma deemed the evidence ‘inadequate’.38 Guidelines take a pragmatic view, advising that exercise and weight loss be part of a general approach to improving lifestyle in patients with asthma.4
Breathing exercises
Physiotherapist-taught breathing exercises tend to focus on managing hyperventilation.39 Individual studies have shown them to reduce symptoms and improve quality of life, but not to improve lung function.40,41,42A Cochrane review called for more trials.43 Breathing exercises may be an ‘adjuvant to pharmacological treatment’ in appropriate patients.4
Dietary modification
On the basis of in vitro and observational studies, dietary supplements including fish oils,44 antioxidants45 and probiotics46 have been proposed to potentially improve asthma control. Trials have failed to show clinical efficacy.4 Although a correlation between high fruit and vegetable intake and better pulmonary function tests has been noted,47 there is no evidence that increasing fruit and vegetable intake improves asthma symptoms.
Dr Andrew Menzies-Gow is a consultant in respiratory medicine at the Royal Brompton Hospital, an honorary senior lecturer at Imperial College London and chair of the NICE asthma guideline development group. Dr Claire McBrien is a specialist registrar in respiratory medicine.
Competing interests: Dr Menzies-Gow has attended advisory boards for Novartis, Astra Zeneca, Teva, Hoffman La Roche, Glaxo SmithKline and Boehringer Ingelheim. He has attended international conferences with Astra Zeneca and Boehringer Ingelheim. He has received lecture fees from Novartis, Hoffman La Roche, Teva, Astra Zeneca, Vectura and Boehringer Ingelheim. He has consultancy agreements with Astra Zeneca and Vectura
Dr McBrien has attended an international conference with Boehringer Ingelheim
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens












