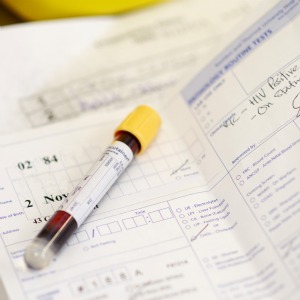
GPs in areas of extremely high HIV prevalence have been advised to consider offering tests to anyone attending a routine appointment, potentially leading to millions more tests under new NICE guidance.
The guidance also recommends GPs in areas of high prevalence offer HIV testing to all patients registering with the practice or undergoing blood tests for an unrelated reason.
NICE estimates that 3.7 million people live in areas of very high prevalence – covering 18 London boroughs, Manchester and Brighton and Hove – while a further 7.9 million live in areas of high prevalence.
GPs welcomed the new guidance, released on World Aids Day, but emphasised that GPs are under no obligation to offer this as it is not part of the GP contract.
Previous guidance specified testing men in areas with high prevalence of HIV or men registered in a practice with a large population of men who have sex with men.
However, the new guidance said that all patients should be offered the test.
It said: ‘In areas of high and extremely high prevalence, also offer and recommend HIV testing to everyone who has not previously been diagnosed with HIV and who: registers with the practice or; is undergoing blood tests for another reason and has not had an HIV test in the previous year.
‘Additionally, in areas of extremely high prevalence, consider HIV testing opportunistically at each consultation (whether bloods are being taken for another reason or not), based on clinical judgement.’
NICE defines areas of high prevalence as local authorities where there are 2-5 diagnosed infections per 1,000 patients aged 15-59, and extremely high as 5 or more per 1,000.
This includes 18 London boroughs, including Lambeth, which has a prevalence of 14.6 per 1,000 patients aged between 15-69 – the highest in the country.
Dr Andrew Green, the prescribing lead for the GPC, said: ‘I fully understand and support efforts to improve the early diagnosis of patients who have been infected with HIV. Early treatment dramatically decreases infectivity and improves survival, and a co-ordinated approach is clearly important.
‘However, the challenge now is on commissioners to provide this service, because screening activities are not part of essential GMS contracts and so GPs are not required to undertake this activity personally, whatever NICE may say. Indeed, they should not do so if it would harm the care of other patients. Many of the practices with high prevalence rates will be in inner city areas who will have high list-turnovers and will already be struggling to provide effective care.’
RCGP cinical lead for HIV, sexual and reproductive health, Dr Philippa Matthews, said the college welcomed the guidelines.
However, she added: ‘As the guidelines acknowledge, there are barriers for GP surgeries to offer wide-scale HIV testing. Funding for such initiatives is currently decided by local councils, and there is no uniformity across the country. There is also the issue of effective implementation – including training and support for practices to adopt these schemes.
‘Furthermore, there are sensitivities that GPs need to take into account when offering HIV tests to patients who are usually visiting the GP for reasons not connected with HIV; a conversation that is difficult within the frustrating constraints of the standard 10-minute consultation. Despite this, many doctors and nurses in high prevalence areas are doing an incredible job at integrating HIV testing into relevant routine care.’
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens