Head and neck clinic – recurrent oral ulceration
An otherwise fit and healthy 31-year-old lawyer presents to her GP with a two-year history of painful oral ulceration. Over the previous six months she has had numerous episodes, in various areas around the mouth. The pain is significant, often interfering with eating, drinking and speaking when they occur. She does not gain any relief from the over-the-counter gels she has been using.
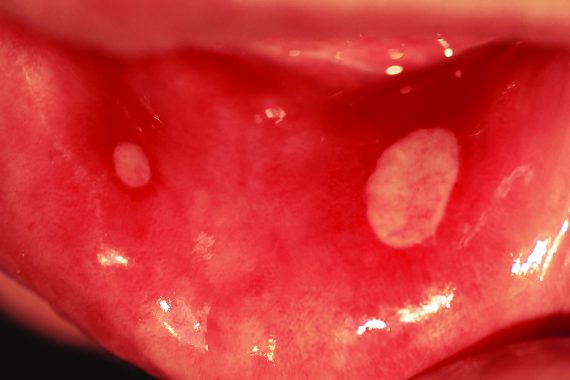
On examination, there are four oval, yellow ulcers on the right buccal mucosa, each around 5mm in diameter. There is no cervical lymphadenopathy. Routine blood tests including FBC, ferritin, B12, folate and ESR are unremarkable.
A diagnosis of recurrent aphthous ulceration is made and the patient is treated symptomatically with chlorhexidine mouthwash and steroid pellets.
The problem
Approximately 50% of the population will be affected by recurrent oral ulceration at some stage. Recurring ulceration can be associated with systemic autoimmune diseases, including mucocutaneous conditions such as pemphigus vulgaris, bullous pemphigoid, Behçet’s disease, erythema multiforme and Stevens-Johnson syndrome. Alternatively, it can occur without an identifiable cause, where it is often classified as recurrent aphthous stomatitis (RAS). Many aetiological factors have been implicated in RAS, such as nutritional deficiencies, anaemias, stress, food allergies, drugs and hormonal changes. The wide range of potential causative agents, coupled with a GP’s limited exposure to intra-oral mucosal pathology, mean the diagnosis and management of recurrent ulceration can be a significant challenge in general practice.
It is important to exclude potential malignant pathology, establish a diagnosis and instigate an appropriate management plan.
Onward referral to local oral and maxillofacial units is often warranted for further assessment and input into management where the diagnosis is unclear.
Features
Recurrent ulceration is typically painful, leading to difficulty eating, drinking and sometimes talking. Ulcers erupt in different areas in the mouth and sometimes patients get a tingling feeling a day or two before the ulcers appear. It is classified into three categories: minor, major and herpetiform ulcers.
The commonest form is the minor variety, where crops of up to five ulcers, no bigger than 10mm (and usually 4-5mm), occur on non-keratinised intraoral mucosal surfaces such as the labial (inner lip) and buccal (inner cheek) or the lateral borders of the tongue. They tend to resolve over a two-week period, healing without a scar.
Ulcers with scarring
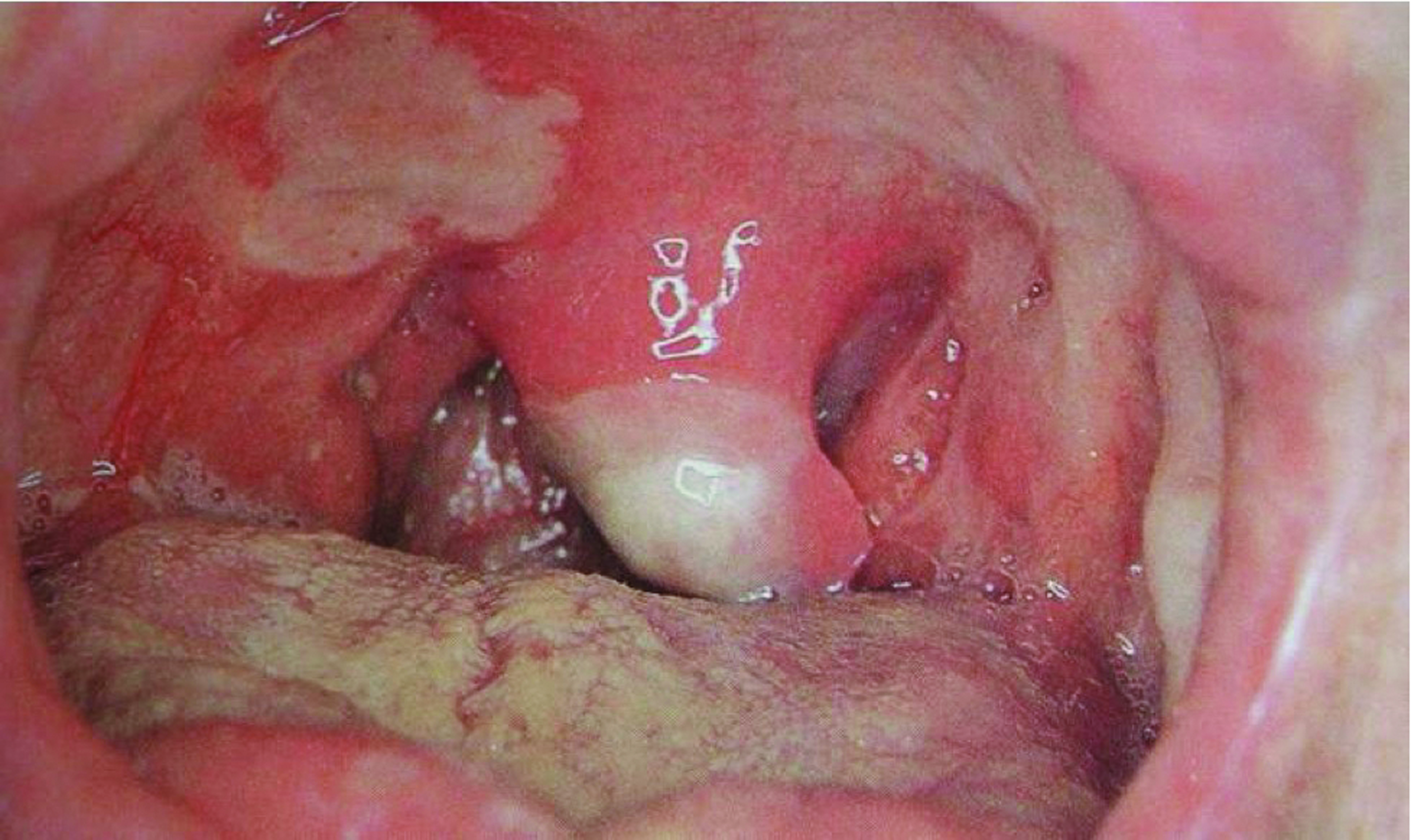
Major ulceration occurs with crops of up to three larger ulcers (10mm or larger), which can occur anywhere in the mouth. They often take up to three months to resolve, leaving mucosal scars. The third variant, herpetiform ulceration, involves many small (1-2mm) ulcers occurring in crops. These ulcers often coalesce, leading to larger, irregularly shaped lesions, which resolve without scars over a two-week period.
Diagnosis requires a detailed history to establish the clinical pattern as well as potential causative factors. A thorough examination of the oral cavity is also required – appropriate lighting and a wooden tongue spatula is generally sufficient to visualise the various mucosal surfaces in the mouth.
Investigation
Complete investigation of recurrent ulceration can be difficult in primary care. Simple blood tests can reveal underlying haematological and nutritional deficiencies. Trials of changes in diet, medication or even toothpaste can also lead to important diagnostic information, but it is important to realise that such tests should not delay onward urgent referral if there is potentially sinister pathology.
Diagnosis
A diagnosis is made clinically in the practice setting. However, when required, ulcers can be biopsied in secondary care, enabling the full remit of pathological evaluation. These ulcers are always soft on palpation, in contrast to most malignant ulcers, which are firm and indurated.
Management
Management of recurrent ulceration in primary care involves correction of any nutritional or haematinic deficiencies. Potentially causative agents can be explored in detail and excluded on a trial basis.
Any underlying causes can be treated, with onward referral to appropriate medical teams if required. However, it is important to remember that, as mentioned above, these processes should not delay the urgent referral of a suspicious ulcer.
Ulcers themselves are treated symptomatically. Over-the-counter topical gels can provide some relief, as can anaesthetic mouthwashes such as benzydamine hydrochloride or chlorhexidine.
Simple steroid pellets such as hydrocortisone buccal 2.5mg four times a day or steroid mouthwashes (betamethasone 500µg in 20ml water used for two minutes twice a day – but tell the patient they must spit this out after use) can also be of benefit in reducing ulcer size, limiting pain and speeding up healing.
Minor recurrent ulceration can usually be treated in the community, although the other variants may require referral for consideration of more significant treatment, such as intralesional steroid injections, systemic steroids or even immunosuppressant therapy.
Mr Arpan Tahim, Mr Karl Payne and Mr Alex Goodson are specialty registrars in oral and maxillofacial surgery at University College Hospital, London, and Professor Peter Brennan is a consultant maxillofacial/head and neck surgeon at Queen Alexandra Hospital, Portsmouth
The authors have recently published a book (Important Oral and Maxillofacial Presentations for the Primary Care Clinician), which has been sent to every GP practice in the UK free of charge. It contains algorithms providing guidance for the management of many head and neck conditions, including neck lumps and malignant disease. The book has been written in collaboration with the RCGP. Further copies are available at cost price (£12.50) from Amazon.
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









