
Five years ago, GPs were placed at the forefront of the Prime Minister’s personal mission to increase the number of people diagnosed with dementia.
The aim was to diagnose two-thirds of the 670,000 people estimated to be living with dementia in England at the time.
A contract was imposed that diverted GP funding into a ‘case-finding’ enhanced service that saw large numbers of patients with vascular disease or diabetes screened for memory problems.
And, on the face of it, this proved remarkably successful, with diagnosis rates increasing from a national average of 42% to around 67%.
After achieving its aims, the DES funding will be withdrawn from next month, but a Pulse investigation can now reveal the extent of the unintended harm that may have been caused by the pressure on GPs to refer.
Figures obtained from 11 NHS trusts showed 152% increase in the number of patients wrongly labelled as potentially having dementia under the diagnosis drive, causing them unnecessary anxiety and affecting the GP-patient relationship.
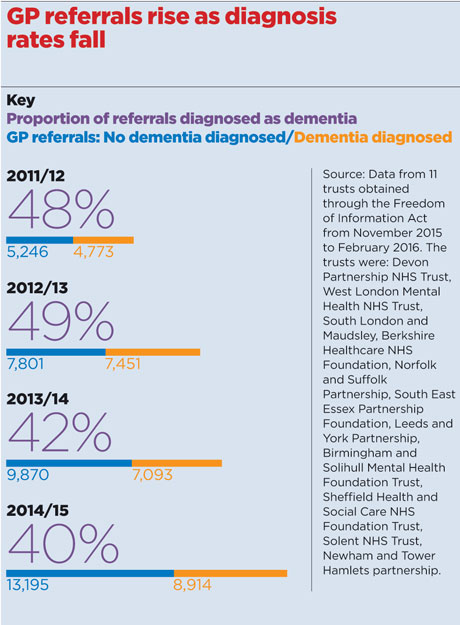
These data, obtained under a Freedom of Information request, reveal there were 10,019 GP referrals across 11 trusts in 2011/12, when the Prime Minister launched his ‘challenge’ on dementia, and that this more than doubled to 22,109 in 2014/15.
The number of diagnoses rose by 87% but the proportion of ‘false alarms’ also rocketed, with 60% of those referred found not to have dementia in 2014/15, compared with 52% in 2011/12.
When GPs originally warned that memory clinics would be overwhelmed, health secretary Jeremy Hunt accused them of ‘grim fatalism’ for ‘refusing’ to recognise the importance of diagnosing dementia.
But the data from trusts show that although the average waiting time for an assessment has fallen, it is still 11 weeks – way above the Government target of six weeks – with some waiting as long as 30 weeks to be seen.
GPs say this has led to a prolonged period where patients have to live with the distress caused by a potential dementia diagnosis, as well as raising hard questions about the poor accuracy of GPCog, the assessment tool recommended by the DES.
Dr John Cosgrove, a GP in Birmingham and a RCGP Council member, campaigned against the introduction of the dementia screening enhanced service and says the Pulse figures show that many of the patients being referred ‘shouldn’t really end up in a memory clinic’.
He says: ‘If the diagnosis rate is going down like this, there are a lot of people who are worried about their memory, whose anxiety is being reinforced from being referred to a memory clinic, only to end up being reassured.
‘You can imagine how anxious you’d be waiting for a memory clinic referral for, say, three months to find out you haven’t got dementia.’
Dr Martin Brunet, GP in Surrey and leading critic of the dementia diagnosis drive, says it is ‘good to see the original DES has been dropped’.
But he adds: ‘As with many targets, once the Government has hit them and the focus shifts onto something else, we will never know how many patients will have benefited or been harmed by these initiatives – there was no plan by the DH to evaluate their effects, and never any acknowledgement they might do harm.’
‘Tsunami of worried patients’
Pulse’s investigation reveals some of this potential harm. Norfolk and Suffolk NHS Foundation Trust showed one of the largest increases in referrals of people without dementia, with 74% of patients referred in 2013/14 found to be false alarms. In 2011/12, this figure was just 51%.
Dr Tim Morton, chair of Norfolk and Waveney LMC and a GP in Suffolk, says GPs saw a ‘tsunami surge of worried patients’ following the campaign launch.
He adds: ‘With screening like that and in these days of risk-averse medicine, GPs are inevitably more likely to refer people on – and with the workload pressures we’re under that will be exacerbated.’
The dementia drive proved controversial from the start – Pulse published a front-cover feature asking whether the DES would prove to be ‘cruel or kind’ – and this disquiet turned to outrage after NHS England rushed through a short-term scheme in late 2014 to pay practices £55 for every new dementia diagnosis.
But the drive has proved effective. The Prime Minister’s challenge set targets to ramp up diagnosis rates from the national average of 42% to that in ‘best performing’ CCGs of around 67%.
And the Department of Health claims this has been achieved. A spokesperson told Pulse: ‘We have made huge improvements. From 42% in 2010 to 67% today – our diagnosis rates are now among the best in the world.’
Professor Alistair Burns, NHS England’s national clinical director for dementia, says patients ‘reporting symptoms to their GP have a right to be investigated regardless of the final diagnosis’.
He adds: ‘The number of people receiving a dementia diagnosis has increased significantly, which is testament to the hard work of GPs in identifying early the signs of dementia and referring patients for assessment.’
But Professor Burns’ statement failed to address concerns about harm caused to patients. And the figures Pulse has may be an underestimate, as a letter in the journal Age and Ageing last year revealed.1
Devastating
Neurologists in Sheffield warned of potentially ‘devastating’ consequences for patients as more than half (52%) of those referred for confirmation of a dementia diagnosis after the introduction of the case-finding DES in the 2012/13 GP contract had psychiatric or functional memory problems, but not dementia. This compared with 25-30% previously.
Dr Daniel Blackburn, consultant neurologist in Sheffield and an honorary senior lecturer at the University of Sheffield, tells Pulse: ‘If memory clinics were 100% accurate and people were seen promptly then you could say there is no real harm. But the falling diagnosis rate of dementia diagnoses made in specialist clinics reinforces our concerns that we are increasing people’s worry about non-pathological every-day memory lapses.’
He adds: ‘In the past I am sure many GPs would have said, “I’m not sure, I’ll see you in six months” – but now, especially if they are incentivised, they may just refer.’
NHS England has claimed that the reason for dropping the dementia DES is a ‘recognition of the fact that GPs are more routinely diagnosing dementia’.
But GPC chair Dr Chaand Nagpaul is scathing, labelling the DES a ‘deeply unpopular and imposed’ service.
He adds: ‘We warned the Government that imposing a scheme designed to meet a political target would distort clinical priorities and have an adverse impact on memory services and individual patients.’
It seems he has been proved right.
Reference
1 Bell S et al. A diagnosis for £55: what is the cost of government initiatives in dementia case finding? Age Ageing, online Jan 2105. tinyurl.com/dementia-warn
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens















