Should everyone be on vitamin D?

Government advisers are expected to call for everyone to have their vitamin D levels boosted later this year, in a radical move that could have major implications for general practice.
But their recommendations will come as many experts are worried about the current rocketing levels of prescriptions for vitamin D supplements.
A Pulse investigation finds that prescribing by GPs has risen 40% since 2012, with the annual cost now £85m.
GP requests for vitamin D testing – costing £20 a pop – have increased by up to 115% in some trusts. This has led some GPs to say prescribing is already ‘out of control’ and is costing millions in GP and nurse time, with little discernible benefit in many cases.
The Scientific Advisory Committee on Nutrition – which advises Public Health England and other government bodies – will make a final decision in the next few months on its ‘precautionary approach’ recommended in draft guidance last year.
The SACN said it was ‘not possible to identify’ those who did not synthesise enough vitamin D in the summer. It concluded: ‘Since it is difficult to achieve the RNI/Safe Intake from natural food sources alone, it is recommended that consideration is given to strategies for the UK population to achieve the RNI of 10µg/d for those aged four years and older and for younger children to achieve a Safe Intake in the range 8.5-10µg/d at ages 0 to < 1 year and 10µg/d at ages 1 to <4 years.’

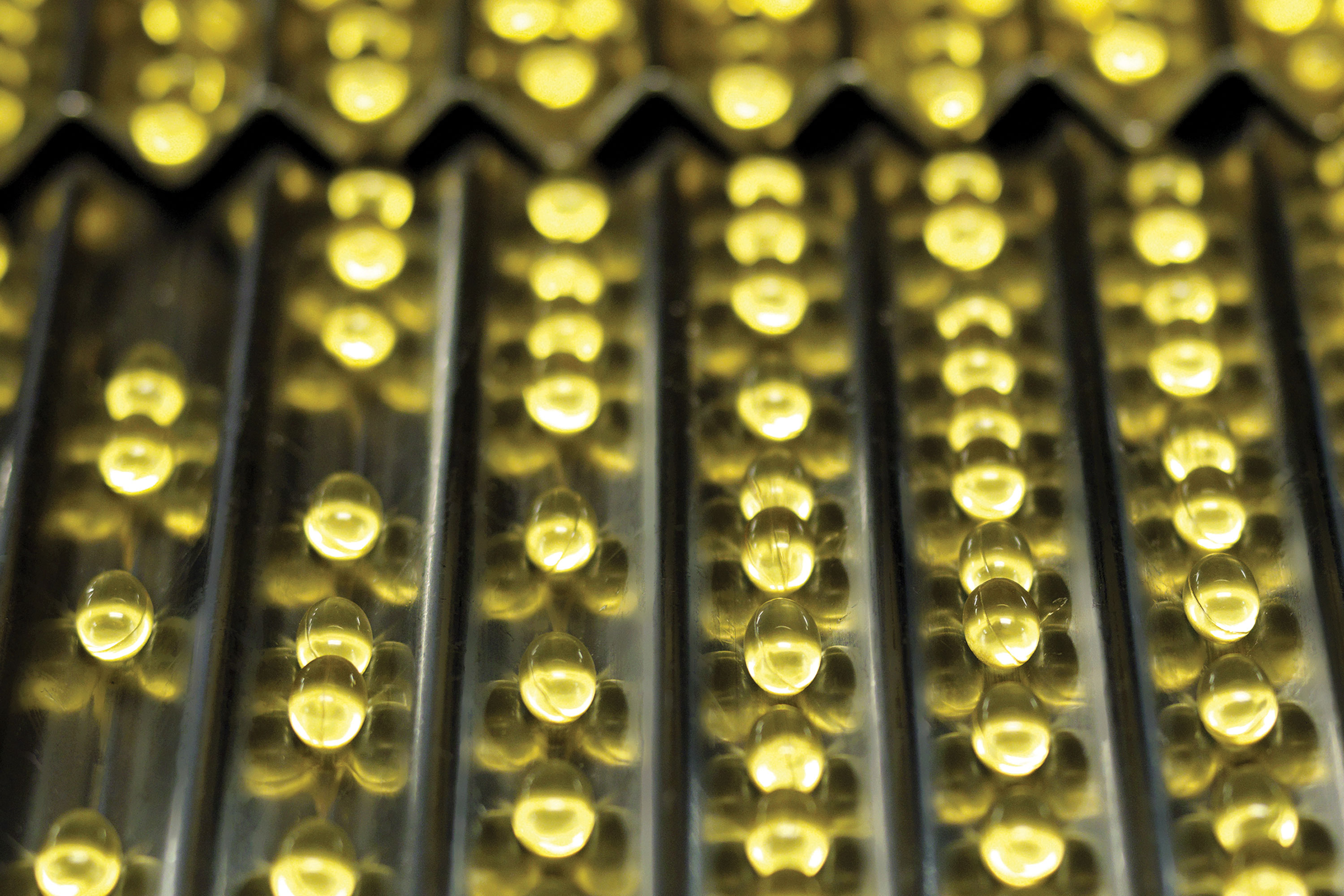
vitamin d box 780x346px
It remains unclear what these ‘strategies’ could entail. But experts say GPs should not bear the brunt of the Government’s vitamin D crusade, and that public health approaches, such as food fortification or boosting the time children spend outside, are needed.
In 2012, the chief medical officers from every UK country made the unusual decision to write to GPs urging them to offer vitamin D supplements to vulnerable groups, including under-fives, people over 65 who are not exposed to much sun, pregnant and breastfeeding women. They stressed that other groups were at risk of deficiency, including people ‘confined indoors for long periods’ and those of African or Asian origin.
We need to prescribe when clinically indicated – not to just treat a blood test result
Dr Alun Cooper, a GPSI in osteoporosis
The letter stressed: ‘As health professionals, you can make a significant difference to people’s health’. This was followed by NICE guidelines in 2014 backing the CMO advice.
All of this has had a powerful effect. An analysis of NHS prescribing data since 2012 carried out by Pulse revealed prescriptions for vitamin D went up 16% in a year following the letter from the CMOs. And, in total, the amount of vitamin D prescribed by GPs has increased by around 40% from 14 million items in 2012, to 20 million items in 2015.
The cost to the NHS has shot up accordingly, from a stable cost of around £4.8m a month before 2012 to £7.1m in the latest figures from last November.
It is not just prescribing that is intensifying. Data from trusts obtained by Pulse under the Freedom of Information Act show the number of tests for deficiency carried out has more than doubled.
‘Out of control’
Barking, Havering and Redbridge University Hospitals NHS Trust said it performed 73,000 tests in 2015 – a 115% increase on 2012. County Durham and Darlington NHS Foundation Trust reported a 95% increase in that time, while Central Manchester University Hospitals NHS Foundation Trust and Trafford Hospital reported a 60% between 2012 and 2015.
Dr Alun Cooper, a GPSI in osteoporosis in Sussex and a member of the National Osteoporosis Society Scientific Committee and the National Osteoporosis Guideline Group, says: ‘The prescribing of vitamin D seems to have gone out of control.
‘We need to prescribe when clinically indicated, for example in osteomalacia, and not just treat a blood test result.’
And the value to patients is a question vexing some leading GPs.

Dr Andrew Green, chair of the GPC clinical and prescribing subcommittee, says he is ‘not surprised prescriptions are rising in the light of increased publicity about vitamin D deficiency’ but warns ‘there has to be some concern that patients are being medicated when lifestyle changes may be more appropriate’.
Other leading GPs have tried to resist jumping on the bandwagon, and remain sceptical. NHS Tower Hamlets CCG, in east London, promotes education in schools and the community to help people modify their lifestyles instead of taking pills.
CCG chair and a GP in the borough Sir Sam Everington says vitamin D deficiency ‘is a marker for lifestyle deficiency, and if you give vitamin D there is a risk you are just biomedicalising it and potentially making the problem even worse, because you’re not dealing with the underlying issue’.
He adds: ‘You’ve got to find systemic solutions – very simple ones, like the amount of time children spend in the playground each day.’
And, despite strong arguments for tackling vitamin D deficiency – notably to combat the worrying return of rickets in children – studies continue to question the benefits and flag up potential harms associated with long-term vitamin D supplementation.
Yet GPs also report being pushed by secondary care colleagues to prescribe vitamin D to non-symptomatic patients with slightly suboptimal levels.
Dr David Mummery, a GP in west London and research fellow at Imperial College London, says this has resulted in ‘massive overdiagnosis of vitamin D “deficiency” over the last few years’.
He says much of this is down to the lack of clarity over the reference ranges for vitamin D. According to ranges applied in his area, where levels below 40-70nmol/L indicate insufficiency, he says ‘over 90% of the UK population’ are likely to qualify for a prescription.
Dr Mummery also cites ‘drug company promotion’ and ‘high patient demand and acceptability’ as major drivers.
With vitamin D tests costing the NHS around £20 each, and GP practices already overstretched, there are concerns about the wider costs to the health service.
Dr Mummery says: ‘It truly has wasted millions of pounds in time, GP and nurse appointments, drug costs and blood tests.’
But some GP experts argue that there is enough evidence linking vitamin D with musculoskeletal strength – and that it is not possible for most people to get enough vitamin D through diet and sunlight, particularly in winter, since 90% of the body’s vitamin D is produced in the skin under exposure to UVB light.
Dr Sally Hope, a recently retired GP who works as an associate specialist at the Nuffield Orthopaedic Centre in Oxford, says she believes vitamin D is still not being prescribed to all those who could benefit.
She says: ‘I don’t think there’s anywhere near enough prescribing in older people. Virtually every person that comes in with a fractured hip to hospital is vitamin D deficient.’
Food fortification
Dr Hope concedes that doubts remain over vitamin D’s role in health but advocates wider prescription.
However, she says: ‘The danger is that, for no harm, you are going to miss those who are deficient – and for example, we know that if women do have very low vitamin D in pregnancy their children’s bone strength never recovers.
‘To say, it’s not important and “why bother” is possibly foolish.’
And if implemented sensitively, the latest SACN recommendations could increase vitamin D levels without overmedicalising people or adding to GPs’ workload.
Some countries, including the US and Australia, already run ‘food fortification’ schemes. Public health advice also promotes vitamin D-rich foods, such as mushrooms, oily fish and dairy.
Dr Mummery says: ‘I think food fortification is sensible and the best way to get vitamin D requirements, along with sensible sunlight exposure advice and also multivitamin drops/tablets.’
This would benefit GPs and the NHS as a whole, he adds: ‘As this should now be routinely advised, expensive testing and “treatment” of supposedly low vitamin D levels can be avoided and save the NHS a lot of time, resources and money.’
However, such campaigns can be subject to ‘nanny state’ criticism. A similar push to add fluoride to the water supply met resistance, so the DH may opt to promote supplements instead. If that happens, patients are likely to seek GPs’ advice and support. And that really would take the sheen off the sunshine vitamin.
‘There is no convincing evidence, except in the severely deficient’

The increase in vitamin D prescriptions raises the concern that many people are prescribed supplements merely because of a finding of a low level of vitamin D in their circulation, with little or no clear symptoms or signs of deficiency.
Furthermore, there is no clear trial evidence to support vitamin D supplementation other than for bone disease in those who are severely deficient, so it may be that many patients do not benefit from being given it.
We must await the results of the VITAL study – a randomised controlled trial of vitamin D3 for the prevention of cancer, heart disease and stroke in 27,000 individuals that is due to report in 2017 – before we can make better informed decisions on widespread vitamin D supplementation in the general population.
For now, GPs should avoid costly testing for vitamin D levels and prescriptions in asymptomatic patients, other than in bone disease-related conditions. While some argue supplementing people ‘to be on the safe side’ is cheap, patients may gain false reassurance from a ‘protective’ tablet.
To improve health and prevent chronic disease we should stick to what is proven: encourage better lifestyles in general and target risk factors in those at elevated risk.
Professor Naveed Sattar is professor of metabolic medicine at the University of Glasgow.
References
1 Prevention of nonvertebral fractures with oral vitamin D and dose dependency. Arch Intern Med 2009;169 (6):551-561 tinyurl.com/jbdef23
2 Maternal vitamin D status during pregnancy and bone mass in offspring at 20 years of age: a prospective cohort study. J Bone Min Res 2014;29(5):1088-1095 tinyurl.com/gn97gqc
3 Theodoratou E et al. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ. 2014: 1;348:g2035
4 Vitamin D and chronic disease prevention. BMJ 2014;348:g2280
5 Monthly high-dose vitamin D treatment for the prevention of functional decline.
JAMA Intern Med 2016;176(2)
6 Vitamin D and bone health. A practical clinical guideline for patient management. National Osteoporosis Society, 2013. tinyurl.com/jhmx9fr
7 Maternal gestational vitamin D supplementation and offspring bone health (MAVIDOS): a multicentre, double-blind, randomised placebo-controlled trial. Lancet Diabetes Endocrinol online Mar 2016.
tinyurl.com/j6yoczt
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









