The stranger prescribing to your patients


prescription cover image 3×2 (1)
It can take just a few clicks for your patient to be given a deadly prescription. And the doctor does not even have to be in the UK.
Richard Breatnach died in Brighton in 2016 after being prescribed more than 120 dihydrocodeine tablets for a migraine. He was able to obtain these tablets by simply filling in an online form, on which he lied about his medical history. His GP was not informed and the prescribing doctor was based in Bulgaria.
The coroner concluded that online prescribing ‘completely undermines the diligent and careful GP’s efforts to control this man’s medication overuse’.
And this case not unusual. Regulators tell Pulse this is one of several deaths linked to online prescribing, and there is growing concern about its safety. GPs will have long suspected this is the case, but regulators are playing catch-up.
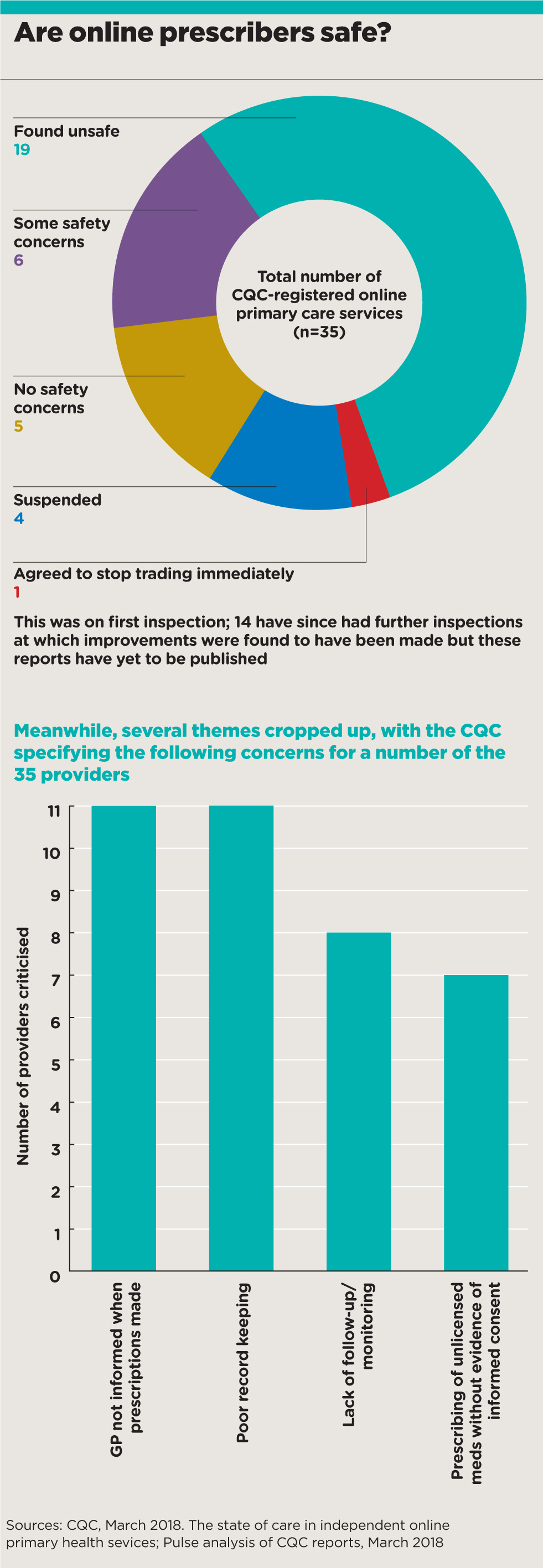
Last week, in response to the concerns, the CQC released a report, which says 43% of the 35 online prescribers it inspected were ‘not providing safe care’ – with some even shut down permanently or temporarily as a result.
It found inappropriate prescribing of painkillers and antibiotics – with the latter handed out to patients who were given the option to choose which one they wanted, at what dose and for how long. The regulator also found over-prescription of asthma inhalers, and use of credit card details as a way of verifying a patient’s identity.
Online prescribing
Even more fundamentally, the CQC report states that online prescribers are ‘not collecting patient information or sharing information with a patient’s NHS GP’ – meaning GPs can’t be sure who is prescribing for their patients. In one case, a provider had failed to share more than 400 patient contacts with GPs. In another instance, ‘opioid analgesics and other analgesics subject to misuse had been prescribed for up to two years without contacting the patient’s GP and with no access to the patient’s full medical record’, the report says.
Pulse has also learned 30 UK-registered doctors are being investigated by the GMC on suspicion of unsafe online prescribing – 19 of them GPs.
The danger also comes from abroad, with the CQC and the Medicines and Healthcare products Regulation Agency (MHRA) both concerned that UK patients can source prescriptions from doctors across Europe.
All this gives the impression of a growing industry that is on the edge of regulation – and GPs are paying the price. As the BMA’s GP Committee prescribing lead Dr Andrew Green puts it: ‘In comparison to the highly regulated world of general practice, these providers seem to work in a “wild west” beyond the reach of many regulators.
‘Of particular concern are prescriptions for drugs with potential for dependence, such as opioids, and for antibiotics, whose overuse threatens us all.’
The RCGP concurs. Chair Professor Helen Stokes-Lampard says: ‘It’s incredibly concerning to hear reports of patients buying prescription drugs online, often from unverified websites, with minimal security checks in place and with decisions being made by prescribers who are unfamiliar with the person they are prescribing for.’
She adds: ‘New services will inevitably experience some teething problems, but when our patients’ health is at risk, urgent, swift action must be taken to comprehensively address these before the service is rolled out further.’
But GPs are often left in the dark about their patients’ prescriptions. A Pulse analysis of CQC inspection reports reveals that at least 11 of the 35 specifically mentioned a failure to share information with the patient’s GP among their criticisms. This included two services shut down by the CQC – Doctor Matt and MD Direct.
‘These providers seem to work in a “wild west” beyond the reach of many regulators’
Dr Andrew Green, BMA GP prescribing lead
Even Babylon Healthcare was criticised by inspectors in its report.
The company initiated legal proceedings that had prevented the initial inspection report being released. It was eventually made available last December, and states that six out of 10 patients prescribed medicines for asthma and four out of five patients prescribed medicines with potential for misuse ‘had not had the details of their consultation shared with their registered GP’.
A Babylon spokesperson says: ‘As reported in December, Babylon was in “the top quartile of most favourable reports carried out by the CQC” and its services were “safe, effective, caring, responsive and well-led”.’
Babylon states on its website that the concerns raised in the inspection relate to patients for whom it was not the primary care provider, and do not apply to its GP at Hand service.
Regulators are making efforts to adapt. Professor Sir Bruce Keogh, NHS England medical director at the time of the inquest into Mr Breatnach’s death, set up a working group following the coroner’s report, involving the GMC, the CQC, the MHRA, the BMA, the Department of Health and Social Care and NHS England to ‘assimilate current regulatory and professional guidance into one place’.
Sir Bruce said this aims to provide ‘greater clarity regarding good practice in respect of online prescribing and supply of medicines’ and give particular guidance around controlled drugs and antibiotics. The working group continues to meet and its work is ongoing.
The issue of overseas prescribing complicates matters, however. The UK is one of only six EU countries to allow prescription medicines to be traded online. This may change after Brexit, but currently any UK-resident patient can sign up to a private online prescribing service in the European Economic Area due to ‘mutual recognition’ of healthcare.
‘There are elements that no one regulates’
Linda Scammell, MHRA senior policy advisor
These services can provide a prescription for the patient to take to a pharmacy, send the prescription directly to the pharmacy, or even send the medication straight to the patient. And UK regulators are powerless to prevent it, providing the company meets the legal requirements for the sale and dispensing of medicines – which are nowhere near as stringent as regulators’ requirements and do not include an obligation to contact the patient’s GP.
MHRA senior policy advisor Lynda Scammell tells Pulse the agency has major concerns about the effectiveness of the regulations and the number of deaths this situation may be potentially causing in the UK.
She says that if the UK chose to go the way of France and Spain, for example, and banned online prescribing, ‘citizens would buy their drugs elsewhere’.
‘It’s too late, that train left the station many years ago and it is in no one’s interest to pull that back.
‘However, it is all about making it a safer environment… no one wants to stifle innovation but there are larger questions around patient safety.’
Ms Scammell adds that a number of coroners’ reports have expressed concern over the risks of online prescriptions.
‘We take this very seriously. [Regulators] have all had to collaborate with each other because we all have defined parts that we regulate and there are elements that no one regulates.’
GPs have no choice but to take this seriously. Dr Bill Beeby, deputy GPC policy lead for prescribing, says: ‘Like many of my colleagues, everything I can think of about it carries the word “risk” and everything it has been sold on is based on convenience. It seems to be based on individuals being able to obtain whatever they desire and there is no way of being able to check whether a patient is telling the story or the truth.
‘We had one patient who was prescribed antibiotics for an infected cyst in a delicate place. Fortunately the patient came in, and it turned out the diagnosis was wrong. There’s probably quite a lot of others who we don’t see and don’t hear about.’
Until the regulators catch up with the technology– if they ever do – you may never know who is prescribing what to your patients until it is too late.
When online prescribing goes wrong
Richard Breatnach
Mr Breatnach died in 2016 after being prescribed more than 120 dihydrocodeine tablets for migraine after filling out an form online. The coroner pointed out that not only was the amount excessive, with instructions given for the pills to be taken every four to six hours, the painkiller should not be prescribed for migraine in the first place. She also noted that no effort had been made to contact the patient’s GP or to check the information he had given.
HR Healthcare, which dispensed the prescription written for Mr Breatnach, told Pulse it fully co-operated with the coroner, adding that it had since ‘ceased dispensing privately issued prescriptions for all opioid medications’.
Doctor Matt
This online prescription service was inspected by the CQC in January 2017 and closed down for six months ‘to protect patients’. Inspectors found a failure to share information with the patient’s GP, and unsafe care, with national guidance ignored and patients at risk of harm due to poor record keeping. Patients were given the option to choose what antibiotic they wanted, at what dose and for how long.
One patient was prescribed an excessive quantity and dose of inhaler for asthma with no diagnosis. Another with red flag symptoms of rectal bleeding and weight loss was not advised to seek urgent medical attention. One patient’s online form was analysed in just 17 seconds. Doctor Matt is no longer registered with the CQC.
MD Direct
When the CQC inspected online prescription service MD Direct in December 2016, its sole clinician was not a GP and admitted they were ‘not competent to carry out the role’. The company agreed to stop trading immediately and no longer exists.
The regulator found patients being prescribed large quantities of inhalers with no follow-up or monitoring despite a ‘serious risk of harm’. The service did not share information with patients’ GPs and unlicensed medicines were prescribed without patient consent or proper records. Medicines for diabetes, Parkinson’s and heart disease, and lithium for bipolar disorder, were all provided with no monitoring and in some cases no evidence of a previous prescription.
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









