Every missed HIV diagnosis is a failure of care
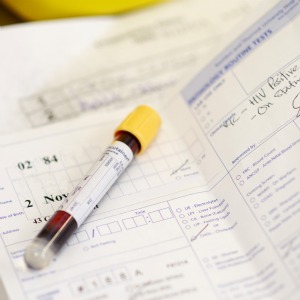
Every HIV diagnosis that is overlooked or missed by any doctor is a failure of clinical care. People whose HIV is diagnosed late have frequently been seen by a doctor prior to their diagnosis without an HIV test being offered.
Nobody dies from being offended, but by overstating the ‘ethical issue’ of offending patients when offering HIV testing, as in your recent article entitled Four ethical issues to consider before offering HIV tests to your patients risks HIV infections being missed or diagnosed too late.
This oversight means that people fail to receive the treatment and care they need which in turn leading to unnecessary illness and in some cases death. HIV testing is important in preventing onward transmission as people who are diagnosed and treated are no longer infectious to other people. NHS Trusts are reporting missed HIV diagnoses as serious untoward incidents and performing root cause analysis on each one. Surely missing a diagnosis of HIV is a greater medico-legal risk to the medical profession than offending someone by offering a test. This article risks reinforcing the HIV associated stigma that we have spent 30 years fighting.
The recent recommendations by NICE and Public Health England to expand GPs remit in offering HIV testing are based on robust evidence that shows an urgent need to increase the awareness and uptake of HIV testing in England. The advice will also help make HIV testing a routine investigation and – we hope – help reduce the stigma that allows HIV to flourish.
HIV currently infects 17 more people each day in England, many of whom will remain unaware of their infection precisely due to the stigma which still clings to this undiscriminating and life-threatening condition. We don’t have a vaccine or a magic bullet, but we could potentially stop nearly all transmission of HIV, nearly all new infections, purely by diagnosing people earlier and putting them on treatment (and by using PrEP), but we are signally failing to do this. More extensive testing, without wasting too much time on risk assessments (which are too often wrong) is the key part of this. This testing cannot be done just in GUM clinics, where there is very little extra capacity, so MUST be done in other settings – particularly in primary care. Without this increased testing, we will never change the epidemiology of HIV in the UK, and every year there will be another 6,000 new diagnoses.
We believe that GPs are perfectly capable of negotiating complexity in all areas of their practice as well as understanding the critical importance of HIV testing. Let’s not reduce the impact of the NICE guidelines that clinicians are expected to follow to deliver best outcomes within safe, competent practice by adding our preconceptions.
Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.












