Investigation: The luxury goods purchased with NHS money


Personal health budgets are NHS England’s new obsession. Managers are travelling the country urging CCGs to sign up more patients to the scheme, which sees patients given NHS cash to spend as they wish.
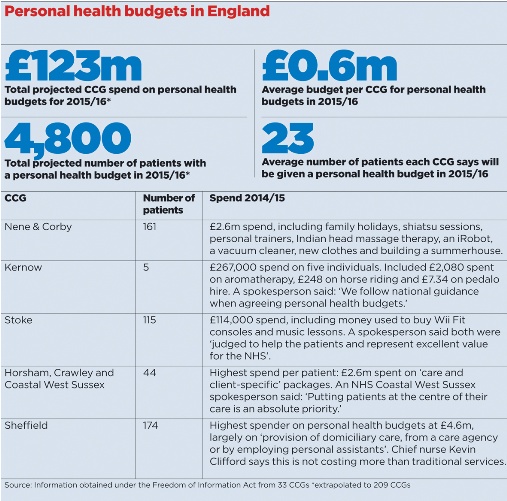
But there are serious doubts about what it is achieving. A Pulse investigation reveals that CCGs are projected to spend £123m on personal health budgets this year, and that patients on the scheme have already been using them to buy a bizarre range of ‘treatments’. The budgets have been used to buy aromatherapy, singing lessons and Wii Fit computer games consoles. Other patients have even been allowed to purchase summerhouses, holidays and hire pedalo boats with NHS cash.
Local NHS managers say these purchases help patients and are ‘excellent value for the NHS’, but they have been criticised as a move towards a private insurance system that will ultimately lead to cuts in useful services and harm patients. And Pulse has learned that personal health budgets are beginning to destabilise existing services, with one mental health service having to close its doors due to its funding being ploughed into the scheme.
Since October last year all eligible patients have had the right to hold a personal health budget if they want one. And NHS England is determined to roll the scheme out further. In its Five Year Forward View, it called for a ‘major expansion’ of personal health budgets to additional groups who may benefit, in particular people with learning disabilities, and this month it is holding a series of roadshows for a ‘development programme to support [CCGs] in expanding their offer of personal health budgets in 2015-16’.

But despite this enthusiasm from managers and policymakers, the policy has been plagued with controversy from its inception. Initial pilots for the scheme, launched in 2009, gave patients an upfront pot of money – either as a direct payment or a ‘notional’ budget held by the CCG or other independent party – for them to spend on services as they chose.
An independent evaluation of the personal budget pilots – led by the Personal Social Services Research Unit at the University of Kent – found there was a significant improvement in the quality of life and psychological wellbeing of the patients and a reduction in hospital costs. It also found patients used significantly more non-NHS services as result of using the personal budgets.
Analysis
The evaluation found personal health budgets were cost effective, with a net monetary benefit of between £1,520 and £2,690 for the personal budgets group, compared with the control group, once the additional costs were taken into account. But a subsequent independent analysis questioned the Department of Health’s conclusions from the pilots, warning the scheme cost thousands of pounds more per patient and was ‘wholly inadequate’ to improve care.
Our investigation has revealed that a vast amount has been spent per patient in some regions, with three CCGs spending a combined £2.6m for 44 patients in 2014/15.
Although the bulk of personal health budget cash across the country goes to pay for personal assistants, therapy and care provision, patients are continuing to spend money on non-traditional services as well. NHS Nene CCG and NHS Corby CCG spent a joint £2.55m on personal health budgets for 161 patients in 2014/15. The items paid for from this budget included a family holiday, to allow a patient to ‘re-establish relations’ with their children, a holiday with a dog, a satnav, an iRobot and the construction of a summer house to give a patient ‘their own space’.
As well as this, funds were spent on non-evidence-based services such as hydrotherapy, shiatsu and art classes. A spokesperson from the CCG said it provides the budgets to patients ‘in respect of achieving outcomes that focus on improving an individual’s health and wellbeing and allowing that individual to take control of how those outcomes are achieved. All personal health budgets are clinically agreed and monitored’.
Games consoles
NHS Stoke on Trent CCG patients spent hundreds of pounds on Wii games consoles and more than £1,000 on music lessons for patients, while NHS Kernow CCG saw patients spend £2,080 on aromatherapy in 2014/15, £248 on horse riding and even paid out NHS cash to hire pedalo boats. A spokesperson for NHS Stoke on Trent CCG said: ‘All were judged to help the patient and represent excellent value for the NHS.’
But GP leaders have been scathing about this use of NHS money at a time when the health service faces an unprecedented funding squeeze, with NHS England estimating it needs at least £22bn of efficiency savings by 2020 just to maintain current service levels. Dr Richard Vautrey, deputy chair of the GPC, says: ‘We continue to have real reservations about this scheme and the inappropriate use of scarce NHS money on non-evidence-based therapies. While individuals may themselves value a massage or summerhouse, others will understandably start to question why they can’t also have such things paid for by the state – and that will just fuel demand.’
He adds: ‘It goes against the current situation where CCGs are looking to penny-pinch as much as they can in order to maintain current services. It can also have a very big impact on existing services, because quite often they are working within limited margins and so loss of even a small amount of their income can jeopardise a whole service – this can have serious implications for large numbers of people just based on the whims of a small number.’
And the scheme comes at considerable cost, with CCGs putting aside millions for it. The 33 CCGs that had set a budget for 2015/16 are expecting to spend more than £19.4m between them. Extrapolated across all CCGs, this would work out at an overall spend of £123m for under 5,000 patients.
In 2013, the Nuffield Trust warned CCGs would need to decommission services ‘not chosen by budget holders’ and warned of the risk of ‘market shrinkage’. And it seems these warnings are becoming a reality. In one region, the CCG had to cut a well-functioning mental health service to fund personal health budgets. The Recovery and Wellbeing Centre, a daycare centre in Basildon, closed in May after NHS Basildon and Brentwood CCG diverted funding to develop personal budgets for patients with mental illness.
MIND, which ran the centre, said the change in funding had cost it £140,000 a year – although most of the patients have yet to receive a personal health budget. NHS Basildon and Brentwood CCG said personal health budgets give patients more ‘choice’, and can be spent on services such as gym membership.
But a recent paper in the Journal of Health Services Research and Policy by Professor Nick Watson, professor of health and wellbeing at the University of Glasgow, found that patients who received the budgets had £4,000 more spent on them than others receiving usual care, irrespective of the complexity of their needs, and that there was evidence the scheme may worsen care. For Professor Watson, cost isn’t the only issue. He tells Pulse: ‘The policy fits the current rhetoric – it is very consumerist and individualistic. Looking at the level of resourcing for the project and the evidence it has been based on, I would say it’s at best spurious. I think we are going forward on poor evidence and there is a clear ideological drive behind it.’
Dr Brian Fisher, a GP in south-east London and patient and public involvement lead for NHS Alliance, agrees there is more an a hint of ideology behind the promotion of the scheme.
He says: ‘Is this a step towards “NHS insurance” where you have to top up to get the level of care that you had access to under previous systems? Is it possible to deliver a budget that empowers patients without putting the state in danger?’ He adds that he knows of someone with a severely disabled child who had her social care budget transferred to her: ‘The budget does not equate to the same quality of care she had access to unless she pools budgets with other users.’

This view was borne out by a survey of more than 1,500 patients by the Patient Information Forum earlier this year. It revealed that more than half of patients with long-term conditions feel they would be ‘unable to make decisions’ on spending a personal health budget.
Others say there is a real risk the scheme will only benefit ‘assertive’ patients. But the DH insists it is a responsible use of public money. A spokesperson tells Pulse: ‘It’s right in some cases that patients with chronic ongoing health needs should be able to take decisions about their own care to help improve their quality of life, and personal health budgets can do just that. They are cost-neutral and so do not take anything away from the public purse.’
An NHS England spokesperson said: ‘Personal health budgets are designed to meet identified health needs in ways that give patients more control over the care and support they receive. The spending must be agreed between the individual and the NHS, meet patients’ individual health needs and achieve the desired outcomes. An independent evaluation has shown personal health budgets are cost effective, help people manage their health and improve quality of life.’
Portfolio careers
What is the right portfolio career for you?














