Austerity and what it means for practices
Austerity is already having an alarming effect on the health service, and it is set to get worse. Across the country, there are warning signs that the finances of the NHS are deteriorating fast.
Despite the Government promising an extra £10bn for the NHS in England – with linked budget increases in the devolved nations – all commentators agree on one thing: the NHS across the UK faces a growing black hole in its finances.
NHS England has said its Five Year Forward View will plug the predicted £22bn gap. But, in the meantime, GPs are seeing the corrosive effects of an NHS having to make cuts while desperately waiting for NHS England chief executive Simon Stevens’ remedy to kick in – if it ever does.
Chancellor George Osborne has signalled yet more financial pain for practices by placing a 1% limit on rises in public sector pay.
There are increasing signs of enhanced services budgets being targeted for savings and a Pulse investigation shows rising use of rationing by CCGs, with hearing aids and vasectomies first for the snip.
Even the heretical concept of charging has raised its ugly head, with health secretary Jeremy Hunt backing the principle of fees for missed GP appointments.
The truth is the health service is facing one of the tightest financial squeezes in its history and Five Year Forward View outlines a punishing regime of future efficiency savings.
Huge shortfall
Mr Stevens has said that, if current levels of funding and spend were continued, by 2020 the NHS would face a £30bn shortfall in the funding needed to deliver the same service as now.

He asked for £8bn in money to kick start his plans for more efficient ‘new models of care’ that will better integrate community and hospital services.
In response, the chancellor confirmed an increase in NHS funding in England of £10bn in real terms by 2020-21 in his post-election ‘emergency Budget’.
Some of this is for new initiatives – mainly seven-day working – but the rest is meant to help NHS England deliver at least £22bn in efficiency savings by 2020.
Mr Stevens recently told the House of Commons Health Committee that these savings would come from three areas. The first was better-value procurement by trusts – and the Government and NHS England have already fired the gun on this with an attack on staffing agency fees.
The second source of savings would be more proactive care through reducing emergency hospital admissions and bed days. Encouragingly, Mr Stevens said: ‘It is a no-brainer. If you don’t invest in primary care and community health services then you will see higher rates of admissions.’
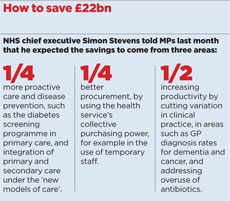
But his third strand was perhaps the most worrying: ‘productivity improvements’. The NHS has consistently been told it needs to make cost-saving measures – most recently through the £20bn QIPP initiative – but has managed just 1% in productivity improvements annually over the past 35 years and is now expected to save 3% a year.
Experts are voicing concern at what could be an impossible challenge for the health service, and the potential effects on patient care if it fails. And GPs are already seeing the beginning of these punishing cost savings.
The chancellor announced in his ‘emergency Budget’ last month that all public sector employees should expect a further four years of 1% pay rises.
GP practices would be lucky even to get that; previous pay awards supposedly giving practices a 1% increase in funding have in fact resulted in year-on-year decreases due to rising expenses.
The downward pressure on GP partner take-home pay looks set to continue.
LES budgets at risk
Meanwhile, LMC leaders are warning LES budgets may be the next to go, possibly under the guise of integrating care.
In Manchester, CCGs have got rid of all enhanced services as part of the move to ‘DevoManc’ – which will see the local authorities and CCGs take control of the whole local health and social care budget.
Manchester LMC leader Dr Tracy Vell says: ‘At this point money is taken away so work has been stopped, for example [enhanced services around] access and heart failure.
‘They have stated it will be replaced by funding for primary care quality standards but there is no agreement yet.’
Other CCGs are cutting enhanced services. A Pulse request under the Freedom of Information Act to 108 CCGs last month revealed that 39 had cut their budgets for 2015/16, while 23 had frozen them at last year’s level.
Northampton LMC chair Dr Jonathan Ireland says CCGs are targeting enhanced services in his area, including axing ‘an access enhanced service to improve GP waiting times and maintain open lists’.
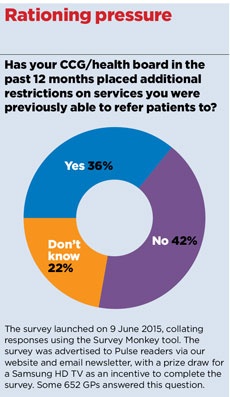
There is also increasing evidence of rationing, with a Pulse survey finding more than a third (36%) of GPs are facing new constraints on services to which they were previously able to refer.
GPs tell us they are finding it harder to refer for surgical treatment of conditions like ganglions or carpal tunnel and, in one area, requests for hysterectomies are simply being ‘fobbed off with a Mirena coil’.
Only two years after coming into existence, 19 CCGs have been ordered by NHS England to devise emergency plans to cut their budget deficits. A Pulse analysis of these recovery plans shows what could be in store for GPs.
NHS North East Essex CCG has a £22m funding shortfall and has had to put in a range of restrictions on vasectomy, female sterilisation and spinal physiotherapy to save £1m. Chair Dr Gary Sweeney explains: ‘We have no choice other than to stay within budget. If we do not implement these decisions we will have to select other services to restrict.’
Hidden pressures
Meanwhile, in a bid to save £1.2m, NHS North Staffordshire CCG will no longer routinely provide hearing aids for patients diagnosed with a mild hearing loss, based on audiometric criteria – a decision labelled ‘cruel’ by campaigners.
But even CCGs that have made the necessary ‘efficiencies’ find themselves in a ‘difficult’ position.
Bristol GP and chief clinical officer of NHS North Somerset CCG, Dr Mary Backhouse, says despite an analysis revealing its services are ‘lean’, the CCG remains 5% underfunded.
NHS Alliance chair Dr Michael Dixon, agrees: ‘CCGs are caught between a rock and a hard place. They try to meet tough budgets and get vilified in the process.’
GPC deputy chair Dr Richard Vautrey says the financial pressure is often hidden. He says: ‘Where patients may have waited three months, they now wait six – this sort of thing is difficult to measure.
‘Until we get new funding into the NHS we will continue to come under financial pressure and it will get worse.’
Austerity NHS
Pay
The chancellor has said public sector workers, including GPs, will continue to receive a 1% pay rise over each of the next four years, although
previous 1% funding awards have in reality left GPs facing a pay decrease due to rising expenses. A Pulse survey has found take-home pay for GP partners plummeted by an average of 4.4% since April. This downward trend looks set to continue.
Rationing
A Pulse analysis of the recovery plans of 19 CCGs with the largest deficits in England shows the kind of measures being taken.
NHS North Staffordshire CCG will no longer routinely provide hearing aids for patients with mild hearing loss. NHS Mid Essex CCG has a ‘restriction policy’ for 2015/16 to save £1m on commissioning of services including acupuncture, facet joint injections and hip and knee operations.
Others are basing restrictions on BMI or smoking. NHS Luton CCG says, ‘when appropriate, patients must stop smoking and/or undergo a weight loss programme’ before certain elective procedures.
Enhanced services
In Manchester, CCGs have got rid of all enhanced services in the run-up to the city-wide integration of health and social care budgets. The LMC says no agreement has been reached about how this will be replaced, although ‘primary care quality standards’ may be introduced. A Pulse Freedom of Information Act request to 108 CCGs last month also revealed 39 had cut their budgets for 2015/16, while 23 froze them.

Charging
Health secretary Jeremy Hunt said recently he had ‘no problem’ with the principle of charging patients for missed GP appointments, but was quickly slapped down by Number 10. But tackling DNAs is on the agenda; a Labour peer mooted an NHS ‘Oyster card’ to penalise non-attenders. In Wales, the Conservatives are pushing for a £10 charge if patients miss a hospital appointment.
‘Prudent’ healthcare
The Academy of Medical Royal Colleges has tasked its members to all come up with five tests or procedures that are of ‘questionable value’. In Wales, ministers are promoting the ‘prudent healthcare’ mantra, with moves to promote lifestyle change over drugs, cutting duplication of work and overtreatment. But Welsh GPC deputy chair Dr David Bailey says Wales is also experiencing cost control ‘via lengthening waiting lists rather than explicit denial of services’.









