Rescue bid for struggling practices – too little, too late?


Two years ago, bosses at NHS England were completely unconcerned about possible practice closures. They told Pulse closures happen ‘all the time’ and were nothing to be worried about.
They are not so relaxed any more.
Managers have been spurred into action after a spate of large closures around the country has destabilised neighbouring practices and thrown the plight of many into sharp relief.
LMC leaders have been warning for years that practices have reached a tipping point, but a Pulse investigation reveals surgery closures have hit a three-year high, with more than 200,000 patients displaced last year. And many others are nearing the brink.
After a year and a half of Pulse lobbying for decisive action, through its Stop Practice Closures campaign, NHS England has finally launched an initiative to support struggling practices.
But the £10m scheme is just a small one-year pilot targeting around 600 of the most vulnerable practices, and GP leaders are warning that it is much too little, too late to reverse the damage being done to general practice.
The pilot aims to parachute rescue teams into at-risk surgeries, offering specialist help with staff, finances and IT. Area teams have been told to come up with lists of practices in trouble, which were due to be submitted by the end of last month. Pulse has learned that in the South-West of England, the area team has identified 17 vulnerable practices covering around 100,000 patients.
If this is replicated across the country then around 620 practices could be in line for extra NHS support worth approximately £16,000 each (enough for a month’s worth of locum cover).
In the devolved nations too, health ministers are realising the extent of the problems in general practice. In Scotland, ministers have committed £60m over three years for practices facing ‘challenges’. In Wales, where several large practices have closed and 10 practices covering 50,000 patients have fallen under health board control, the Government runs a scheme that allows vulnerable practices to apply for support that could include funding, more training or additional staff, such as a practice nurse.
But in England, the situation has been made worse by the time it has taken NHS leaders to acknowledge the true scale of the problem.
Sudden move
Despite NHS chief executive Simon Stevens’ personal stake in expanding general practice – through the ‘new models of care’ in his Five Year Forward View – executives have been slow to develop any scheme to support struggling practices.
The £10m fund for vulnerable practices in England was announced as part of health secretary Jeremy Hunt’s ‘new deal’ last July.
But it was six months before area teams were told to come up with a plan to ensure the ‘sustainability and quality’ of general practice. Guidance issued last December to all CCGs and local area teams says this must address ‘workforce and workload issues’ in general practice in 2016/17.
All regions were tasked to draw up lists of their most vulnerable practices over Christmas using an NHS England ‘vulnerability risk matrix’ and submit them by last week. Practices were scored using measures such as the number of patients per GP, CQC ratings, QOF achievement and the number of sessions not routinely filled.
Pulse understands from instructions sent to area teams that practices that qualify will receive ‘externally facilitated provider support’ designed to build ‘longer-term resilience rather than deliver short-term quick fixes’. This could include financial incentives to help them retain GPs near retirement or adapt clinical roles to allow GPs to spend more time with complex patients.
The details are still being finalised, but it appears NHS England is using as a model a small scheme that began in the South region last July. This scheme appointed 21 organisations, including superpractices, foundation trusts and three private companies – among them corporate giant Virgin Care – to assist struggling practices.
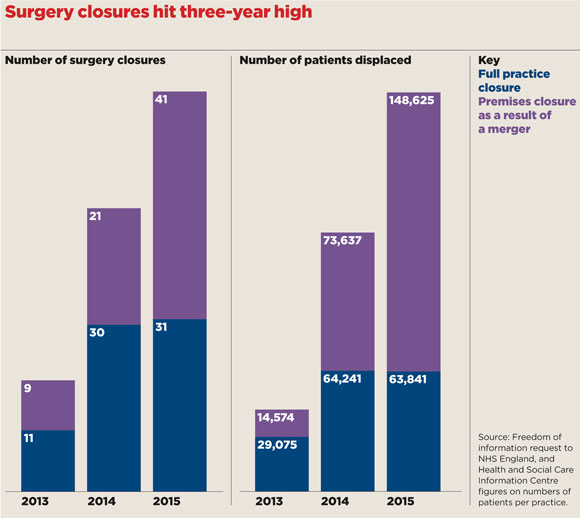
practice closure graph 580x518px
Tipping point
But GP leaders warn many practices have shifted into the ‘vulnerable’ category over the past year, due to ongoing funding cuts, and workload and recruitment problems. Pulse has learned a number of practices are intending to hand back their contracts in April, including two practices with in excess of 10,000 patients hit by PMS funding cuts.
GPC chair Dr Chaand Nagpaul tells Pulse the £10m fund is ‘far too low’. He adds: ‘It’s only going to be targeted at a small number of the worst-affected practices, while ignoring the iceberg underneath – the large number of practices reaching their tipping point.
‘What we really need is proper resourcing if we’re not to continue seeing more and more practices becoming unsustainable.’
Dr Nagpaul says he has advised NHS England that there should be funding for ‘resilience teams of GPs, practice managers and nurses’ to support practices going through difficulties.
He adds: ‘We shouldn’t be waiting for a crisis, we should be trying to prevent it and that needs much more than £10m.’
The NHS England scheme expects practices that receive support to contribute matched funding on a 50:50 bases as a ‘measure of their commitment to improvement’ – a stipulation GPC deputy chair Dr Richard Vautrey describes as a ‘big issue’ for the effectiveness of the scheme.
Dr Vautrey says: ‘Even if you were to identify practices that might benefit from support, would they be willing to accept that, bearing in mind they’d have to find 50% of the funding? That has to be recognised as a big constraint in being able to support the right practices.’
Many practices may be unaware that they will qualify for additional funding. The Victoria Park Practice in Bridgwater, Somerset, is on the risk list, but had no idea of this until contacted by Pulse.
Practice manager Paul Cawkwell says: ‘We are in one of the most deprived areas of the country and our PMS premium funding used to pay for an extra doctor. NHS England is not doing anything to sustain us; they are taking money off us.’
In some areas NHS managers have asked practices to apply for the funding, but with a challenging timeline. Nottingham GP Dr Hussain Gandhi says his practice heard about the scheme just days before the deadline: ‘We were contacted about the scheme, but receiving the information just a few days before the deadline meant applications were rushed.’
Many LMCs have not been consulted about the scheme and have little idea about which practices will benefit. But Dr Peter Graves, chief executive of Bedfordshire and Hertfordshire LMCs, tells Pulse he has been able to work with the area team to push forward incentives the LMC has developed to get retired GPs back into practices and a diagnostic tool to enable early identification of struggling practices so they can be assessed and given appropriate support.
But Dr Graves is not convinced £10m will in itself make much difference: ‘I honestly don’t believe pumping a bit of money into one particularly vulnerable practice is going to have a long-term effect. Potentially it will just stave off the moment of truth and cause a bigger impact on local practices when that moment comes.
‘We’re trying to make sure this money is being utilised in a way which is more sustainable.’
Many practices in trouble will hope he and others succeed.

mission implausable map 780x980px
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens












