Thousands more ‘fit notes’ issued – but one in five GPs say their advice is ignored
Exclusive GPs are issuing more so-called ‘fit notes’ than ever for patients, but a Pulse survey reveals that many say the advice written on them is often ignored by employers.
There have been several recent attempts to cut back on the burden of GPs filling in statements about whether patients are fit for work, but the latest available figures show a 9% increase.
NHS Digital data show 1.4 million fit notes were issued over July-September 2017, compared with 1.3 million over the same period in 2016.
The revised Med 3 was introduced in 2010 and was designed so that GPs could give more advice about what modifications may be needed for patients to return to work, but a Pulse survey of more than 800 GPs found 21% thought employers didn’t usually follow their advice, compared with 44% who did.
The NHS Digital report said that there had been ‘an 8.7% increase in fit notes issued from Q2 2016-17 to Q2 2017-18 where a diagnosis was available’. There was a significant increase in Med 3 forms issued for mental and behavioural disorders (14% rise), while the number of notes that were for five weeks or longer rose slightly, from 34% to 35%.
GP leaders said that this demonstrated the lack of services to help patients recover from mental health problems. The rise also comes despite major moves by the NHS to shift the Med 3 form-filling away from GPs.
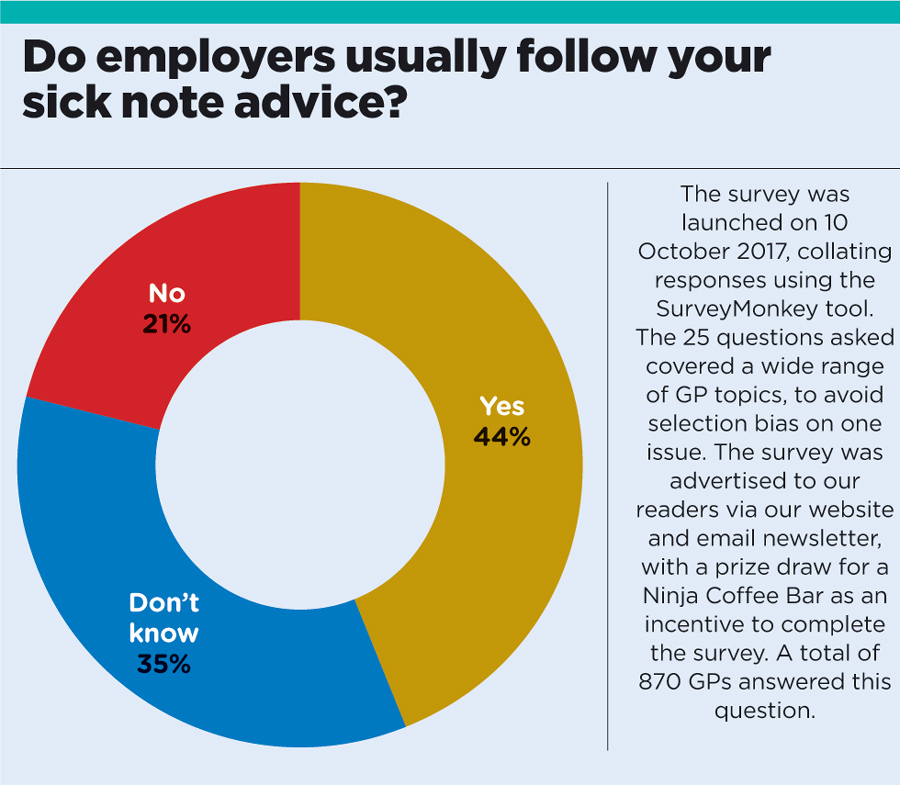
sick note pie chart
Hospitals must now issue fit notes to patients being discharged from their care and covering the entire period until recovery or further clinical review is needed under changes to the NHS Standard Contract 2017-19, which came into effect last April. Also, a new ‘Fit for Work’ service was introduced in England in 2015 for GPs to refer patients who were off work for four weeks or more, although this new service is not widely known.
A Department of Work and Pensions consultation in October 2016 went even further, looking at the extension of fit note certification from GPs to other healthcare professionals, but this has yet to be implemented.
BMA GPs Committee chair Dr Richard Vautrey, said: ‘This is yet another indicator showing the workload pressures GPs are facing as they strive to respond to demand from their patients, and in particular the growing number of people living with stress, anxiety and depression.
‘Despite this, mental health funding has lagged behind, exacerbating the problem. The vast majority of adults with mental health problems are looked after in primary care, but our own research has shown unacceptably long waiting times to access to talking therapies, which can often lead to patients taking longer to recover and further impact being felt in general practice. This is why we need more investment in local mental health therapists and IAPT services.’
Dr Alice Hodkinson, a GP locum in Cambridgeshire, says: ‘I find a lot of employers (and employees) don’t understand how fit notes work, and it takes up a lot of our time for no good reason. Some big companies wanted sick notes after two or three days.’
In June 2016, GPs at BMA’s LMCs Conference voted that fit notes were a waste of clinical time that could otherwise be better spent.
At the time, Merseyside GP Thomas Kinloch said: ‘Fit notes are confusing. Employers, patients and doctors find them confusing. But what do you expect when you call a form issued to cover sickness a fit note? There is absolutely no evidence that fit notes helped early returns to work or reduced overall absence rates and patients still make inappropriate appointments just to get their fit notes in their droves.’
What are ‘fit notes’?
The Statement of Fitness for Work system, introduced in April 2010, applies across England, Wales and Scotland, and provides evidence for employers and for those claiming relevant benefits from the Department for Work and Pensions.
Fit notes (or Med 3 statements) are issued to a patient following seven days of absence from work due to sickness, if the assessor believes the employee’s ability to work is hindered by their health.
The doctor will then categorise the patient as either ‘unfit for work’ or ‘may be fit for work subject to the following advice’. Accompanying notes can also be provided with suggested changes to the role or workplace that will allow them to continue working.
But in June 2016, GP leaders at the LMCs Conference voted that fit notes were a waste of clinical time that could otherwise be better spent.









