Nuclear option: Rise in practices seeking to close or merge

Practices are no longer just thinking about taking the nuclear option – they are actively pursuing it.
Figures obtained by Pulse reveal the stark truth: in a single year, there has been a 500% rise in practices telling NHS managers they wish to merge or close.
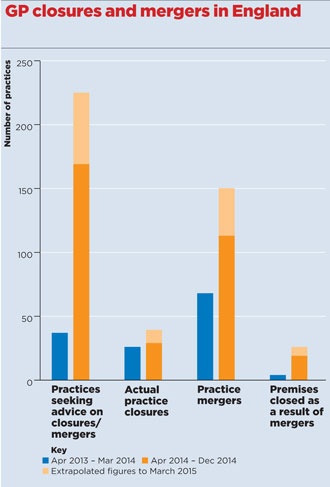
A Freedom of Information (FOI) request by Pulse – made as part of our Stop Practice Closures campaign – reveals a staggering 169 practices in England approached their area team for advice about closing or merging between April and December last year.
Extrapolated across the 2014/15 financial year, this represents an increase of 508% compared with the 37 requests over the whole of April 2013-March 2014.
The FOI request also revealed that 78 practices have either closed completely or closed a branch surgery as a result of merger since April 2013 – a trend that has accelerated since April 2014.
LMCs say their time is increasingly devoted to the growing numbers of practices who are considering closure. And in many cases, area teams are unable – and sometimes unwilling – to provide the support practices need to survive.
The GPs involved say they’re in an impossible situation, caught between continuing in an unviable practice and their reluctance to let patients down.
And there is a significant knock-on effect on neighbouring practices, who can be overwhelmed by an the influx of patients whose practice has just closed.
A cocktail of problems has led practices to take this difficult decision: NHS England is refusing one in three requests to close practice lists; the withdrawal of MPIG is seeing hundreds of practices lose funding worth £3 per patient each year; PMS reviews are removing vast chunks of funding of up to £400k from practices; and many simply cannot recruit enough new GPs to cope with crippling workload or replace partners who are retiring in greater numbers.
Dr Robert Mockett, a GP partner in Brighton, was forced to close his Eaton Place Surgery on 28 February as he and his partner are retiring and could not find anyone to take over the surgery. They had to sell the practice to pay the mortgage, redundancy packages and other costs.
Related stories
GP closure: ‘This is like a bereavement’
In full: GPC guide to managing workload
GPs offered £25 per patient they register after practice closure leaves thousands without a GP
Dr Mockett told Pulse two days before the practice closed: ‘The outpouring of emotion from patients has had me in tears all morning.
‘I thought I’d stay until 65 but I would not survive. I feel for my patients.’
Dr Peter Maksimczyk, a GP in Weston-super-Mare, Somerset, is in the ‘very sad’ situation of potentially having to sell his surgery because he can’t find anyone willing to take it on in the current financial climate.
He says: ‘We have a nice, traditional practice with high patient population. I am 64 and still working full time; my partner is slightly younger. In the next few months, I will be seeking to retire, or at least drastically reduce my commitment, but am concerned that no one will want to take on the practice.
‘If that is the case, I will have to sell up and convert the surgery into flats, which would be very sad. I’m certainly not going to carry on doing what I am now.’
There is a feeling among GP leaders that we have reached a tipping point in terms of sustainability of general practice in many areas.
Dr Robert Morley, chair of the GPC contracts and regulations subcommittee, says: ‘This writing has been on the wall for the best part of a couple of decades and is now painted in enormous bold capital letters in a fluorescent font with powerful searchlights pointed at them.’
In London, the area team received 33 requests from practices in need of support between April and December 2014, compared with 12 in 2013/14.
Londonwide LMCs medical director Dr Tony Grewal says this pressure is being felt on the ground. He says: ‘We spend a huge amount of time trying to rescue practices under threat, with variable success I would say.’
Dr Grewal claims the area team is not helping, and that it is happy to let smaller practices go to the wall.
He says: ‘We are facing the difficulty that for practices below a certain list size – certainly less than 4,000 and sometimes more than that – NHS England’s London area team has a default position that they simply disperse, rather than renewing the contract.’
Elsewhere, there is equally scant support from NHS England. In Cumbria, the Hawkshead surgery tells Pulse a perfect storm of problems means it is on the brink of closure, including removal of seniority payments, a fall in permanent patients and spiralling locum costs.
This has led to a funding gap of £30,000 – some 25% of its income – but there is no additional financial support, despite high-level discussions with NHS England’s head of primary care commissioning Dr David Geddes and health minister Earl Howe. Andy Pow, a campaigner for the practice, says: ‘The problem is when the current GPs retire, no one will come in. Why would they?’
But in the South-West, the North Somerset, Somerset and South Gloucestershire area team has been having ‘sensible’ discussions with struggling practices, the LMC says. There were 16 requests for support from practices considering merger or closure last year but none the previous year.
Wider effect
The wider impact of closures is also being felt. A Pulse survey in January showed one in five GP practices had felt the ‘ripple effect’ on workload of taking on additional patients after nearby closures. In Brighton, the local area team acknowledged the problem by offering practices an unprecedented one-off admin fee of £25 per patient, after 3,000 patients were left without a GP following the closure of Dr Mockett’s surgery.
NHS England admits primary care is under severe strain, but says: ‘We are supporting general practice by progressing co-commissioning to help CCGs lead new, integrated pathways of care, and are investing £1bn in a primary care infrastructure fund.
‘We will see a change in the primary care landscape so the profile of practices will change, but we are taking action to ensure all patients have access to high- quality primary care where they live.’
What GPs are saying

Dr Peter Maksimczyk, GP in Weston-super-Mare
[If we are unable to find people to take over the practice] then I will have to sell up, which would be very sad.

Dr Sanjeev Juneja, GP in Rochester
I have to decide whether to work myself to death or walk away and potentially close the practice.

Dr Naomi Beer, GP in Tower Hamlets
I think NHS England is prepared to accept a certain percentage of practice closures.

Dr Harry Yoxall, Somerset LMC chair
There are a number of practices looking at their future, especially in view of the workforce problems.
Dr Tony Grewal, medical secretary, Londonwide LMCs
NHS England does its best. But it simply lacks the financial and administrative flexibility… to support a struggling practice.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens