
The ghost of general practice
Source: © Matt Kenyon
General practice is being promised a different future. Along with the rest of the health service, it is being gifted a long-term plan by the health secretary and NHS England.
Prime Minister Theresa May has committed an additional £20.5bn a year to the NHS by 2023, which will be used to implement what NHS England is calling its 10-year plan.
And, in a break from the past, it seems the Government is serious about increasing investment into general practice. The PM has announced £3.5bn a year will be given to primary and community care – on top of the £2.4bn a year announced in the GP Forward View.
The announcement specifies that there will be new ‘community-based rapid response teams’ – made up of doctors, nurses and physiotherapists – who will provide emergency support closer to patients’ homes. The Government has also announced the rollout of a ‘successful’ pilot that sees teams of healthcare professionals, including GPs and pharmacists, assigned to care homes, including providing out-of-hours care.
‘The status quo is not an option’
Dr Chandra Kanneganti
The details still need to be fleshed out – especially where the funding will go. Yet the whole direction of travel set by health secretary Matt Hancock and NHS England has been clear, and provides major clues about how the money will be allocated. They want a focus on prevention and greater use of technology. They want larger practices. And they want GPs to specialise in chronic diseases, supported by other healthcare practitioners who take on acute cases.
GPs recognise the need for radical change. Worn down by the conveyor belt of 10-minute appointments, increasingly complex patients and lack of clinical staff, they have reached breaking point. They need new ways of working, crucially with sufficient additional funding to deal with rising demand for services. As one says, ‘the status quo is not an option’ anymore.
Primary care networks
Primary care networks, serving around 50,000 patients, are becoming standard. Around half of NHS England’s £508m Sustainability and Transformation Fund, announced in the GP Forward View in 2016, was earmarked for redesigning services, including practices working together at scale.
The Estates and Technology Transformation Programme, part of a £1bn fund, was set up for new premises and IT systems to integrate practices. NHS England said, as of March, 970 projects had been delivered, with 700 in development.
Interim findings from the review of the GP partnership model highlight `increasing collaboration between practices’, claiming 5,000 practices are now part of networks.
What we can expect in the 10-year plan
The PM and health secretary have already announced `rapid response teams’ of doctors, nurses and physiotherapists to provide urgent care in the community. There are few details, but it is a safe bet they’ll be provided by primary care networks.
In fact, it is likely that much of the £3.5bn will go to these networks to provide services traditionally termed `community care’.
In fairness to ministers, the £3.5bn a year – 17% of the total NHS funding uplift – will go some way to addressing the funding discrepancy between primary and secondary care. But it may also be redefining what is meant by primary care – begging the question, is the NHS’s vision the right one for general practice? GPs could be forgiven for greeting the funding with some trepidation.
There is no doubt that some consistent themes are coming from ministers and NHS England. High up the agenda will be the focus on prevention, after Mr Hancock last month revealed his ‘vision’ for the NHS is to shift the focus onto prevention by empowering patients to take more care of their own health.
He said the Government wants a ‘radical shift’ from ‘a hospital service for the ill’ to a ‘nationwide service to keep us healthy, where those on the front line of the NHS, including the GPs who are its bedrock, feel confident to remind people of their responsibilities too’.
This shift will involve more social prescribing, with GPs recommending services such as art clubs, sports or walking groups – as a way to complement medical treatment and help people self-manage long-term conditions.
The use of technology will be pivotal, with GPs’ initial contacts with patients likely to be digital. The health secretary is known to favour this route; he endorsed the national rollout of Babylon’s GP at Hand app, which offers NHS patients a video consultation within hours.
Mr Hancock believes technology can ‘where appropriate, reduce the need for travel and face-to-face appointments’.
The use of technology
It is no secret that health secretary Matt Hancock is a fan of digital technology and wants to see the NHS using more of it, especially in general practice.
Since he is a patient of Babylon’s GP at Hand video consultation service for NHS patients himself ± and has said he would like to see it `available to all’ ± it is clear that the online consultation model is one Mr Hancock favours.
The NHS is due to launch its own app shortly, and it’s already been encouraging GP practices to introduce online consultations through its £45m fund.
What we can expect in the 10-year plan
NHS England medical director, Professor Stephen Powis recently revealed GPs could soon be referring patients to outpatient appointments that will be conducted via Skype in a bid to cut down on unnecessary trips to hospital.
Meanwhile, GPs can also expect more initiatives encouraging remote monitoring ± so they can view a patient’s data in real time ± and more primary care consultations via video or through online forms.
Meanwhile, the NHS’s own app is due to launch this month. It will enable patients to book appointments, check symptoms and order repeat prescriptions. Future updates could also support GP video consultations.
Stoke GP Dr Chandra Kanneganti, the BMA GP Committee’s lead on working with NHS England on investment, says: ‘I imagine the future will look like this: the patient has symptoms, which they put into an app and it tells them to carry out self-care, or that they need to see a pharmacist. Or if a GP is needed they’ll be given access to an online triage consultation – or even the chance to book an appointment.’
Superpractices and larger groupings in general also feature in general practice’s future. There is a shift to primary care networks, whereby groups of practices serve populations of around 50,000 people, sharing workforce and technology. Already, the NHS has given millions of pounds to practices willing to work ‘at scale’ in this way (see below).
‘Why is it not going into core general practice?
Dr John Ashcroft
Family Doctor Association chair and Swindon GP Dr Peter Swinyard says: ‘The way practices have come together in the last year has been quite dramatic.’
NHS England has been incentivising practices to merge, federate and offer secondary care services, and there would be little surprise if the £3.5bn a year is conditional on pursuing this agenda.
Prevention
Prevention will become the focus of the NHS, health secretary Matt Hancock announced last month in his new vision for the health service.
For GPs this will mean increased social prescribing: recommending activities such as volunteering, arts, group learning, gardening, cookery, and sports.
Social prescribing is being seen as a successful way to help patients manage long-term conditions. The Government announced £4.5m earlier this year to fund 23 such services in England, after lobbying by NHS England’s clinical champion for social prescribing GP Dr Michael Dixon.
What we can expect in the 10-year plan
More money for prevention will be key. In his speech on prevention last month, Mr Hancock said that `in the UK, we are spending £97bn of public money on treating disease and only £8bn preventing it’.
GPs will be expected to take on a wider role ± advising patients on non-medical treatments and positioning themselves as public health doctors.
Making social prescribing available in every local area by 2023 is expected to be high on the agenda, as are efforts to reduce childhood obesity and to ensure earlier diagnosis of disease through genome sequencing.
And the role of the GP is to be revolutionised within these large-scale practices. They will specialise in long-term conditions, and supervise nurses and physician associates, who will see patients with acute problems.
pulse november cover 183x231px
At the same time, as last month’s Pulse reported, GPs want greater flexibility in working patterns and the opportunity to hold a variety of roles as part of a portfolio career, instead of being restricted to full-time work in surgeries.
Official NHS Digital figures show the percentage of partners and salaried GPs in England working less than full time has steadily increased from 66% to 69% over the past three years. Working in networks with access to a shared wider workforce gives GPs more time to pursue other clinical interests, according to the initial findings of the Government’s GP partnership review, led by Wessex LMCs chief executive Dr Nigel Watson.
The shift to part-time/portfolio GP working
GPs are already turning to portfolio careers, which offer them a variety of roles alongside their work in surgeries, as Pulse reported last month.
This is often an attempt to cut time in practice to reduce stress and provide a better work-life balance. NHS Digital figures show 69% of partners and salaried GPs in England work less than full time, the highest proportion ever.
What we can expect in the 10-year plan
HEE has launched its latest GP trainee recruitment drive by extolling the flexibility of general practice, so there seem likely to be new schemes to encourage GPs to widen their portfolio of work. As practices work together more opportunities for GPs to specialise may arise.
Scotland is leading the changes in how GPs work. Its 2018 GMS contract repositions GPs as ‘expert medical generalists’ who focus on undifferentiated presentations and complex care, while leading an extended primary care team.
Dr Kanneganti is broadly in favour of these changes, which he says will unlock access to a shared multiprofessional workforce and allow GPs to move away from the ‘risk’ of 10-minute appointments.
‘There has to be a way of working differently,’ he says. ‘The status quo is not an option.’
Yet concerns remain about this general direction of travel. As Doncaster LMC chief executive Dr Dean Eggitt puts it: ‘We are not choosing this because it is the best way of working; it is the best way of working with the resources that we have.’
Dr Eggitt is worried that the GP partnership model won’t survive such changes. He fears there will be a more radical shift to a version of accountable care organisations (ACOs), which will bring together not only general practices but also district hospitals, acute trusts and mental health services – all using the same pot of funding and sharing risk. NHS England consulted on this type of organisation earlier this year but has yet to publish its findings.
Dr Eggitt warns the GP partnership model will largely not survive a shift to ACOs: ‘To enable that, the GP partnership model is likely to die out.
‘This is because it is based on profit from an efficient system. Risk sharing with acute and mental health trusts is not that. Any profit from working together would not be returned to general practice as it is now.’
General practice will instead morph into small outpatient departments or ‘primary care outlets’ run by the bigger parent organisations, he suggests.
The skill mix: GPs becoming `expert generalists’
In the future, GPs are expected to deal predominantly with complex patients ± those who have multimorbidity and long-term conditions ± while a larger workforce of physician associates and nurses will take care of acute on-the-day appointments.
This could involve GPs becoming known as `expert generalists’ ± as is the case in Scotland, where a new contract this year aims to ensure GPs focus on the skilled work only they are trained to do and can pass on more routine tasks to other professionals.
There have been moves by Health Education England to expand the physician associate workforce ± and the health secretary has recently confirmed those in the role will be regulated in the future.
What we can expect in the 10-year plan
Renewed efforts to ensure 1,000 physician associates are trained for primary care by 2020, as pledged by HEE in the GP Forward View. The latest official figures show just 79 working in general practice as of March 2018.
Funding may also potentially be allocated to train more of other healthcare professionals to work closely with general practice, such as pharmacists and paramedics to assist with prescribing and home visits.
Dr John Ashcroft, an executive officer of Derbyshire LMC, has similar concerns about the redefinition of primary and community care funding. He says: ‘My big problem is that when you start lumping this all together with community, will this money just end up in the community trust?
‘Why is it not going into core general practice? Is it ring fenced? If not, then why not?’
Dr Ashcroft, and many GPs, are worried about how these reforms will affect some of the most fundamental elements of general practice.
He adds: ‘The Government and the Department of Health and Social Care don’t believe in general practice, don’t believe or trust general practice. It’s all about supporting work at scale, but the other side of the coin is they don’t understand what traditional general practice can do with continuity of care. We need more of that and not less.’
Dr Swinyard says: ‘We will have a fight on our hands to try to preserve the essential part of general practice, which is the lifelong doctor-patient relationship.
‘We will undoubtedly be playing more with email, skype consultations, all the remote-access things which mean people don’t have to speak to a doctor.’
The doctor-patient relationship will also be put under further strain when more consultations are taken on by nurses and physician associates.
Of course, the major elephant in the room – and one of the biggest drivers behind these reforms – is the shortage of GPs. The Government has all but abandoned plans to increase the workforce by 5,000 full-time-equivalent GPs from 2015 to 2020, having lost more than 1,000 FTE GPs in the past three years.
‘It certainly doesn’t go all the way’
Professor Helen Stokes-Lampard
Dr Eggitt says this highlights a fundamental problem with NHS plans for general practice. He notes the new schemes announced under the £3.5bn ‘are extra to the care we already offer’.
‘The [rapid response] scheme itself sounds great – how could we not want care in the community for patients who urgently need it, diverting them away from A&E so genuine emergencies can be seen in the A&E department?
‘But practically speaking, we don’t even have enough doctors and nurses to staff the hours of 8am to 6pm five days a week.’
What the pledged £3.5bn does do is begin to redress the disparity in funding between primary and secondary care. An analysis by Pulse in July revealed the percentage of NHS funding going to core general practice has been falling year on year since 2015/16, to its current level of just 7% (see below).
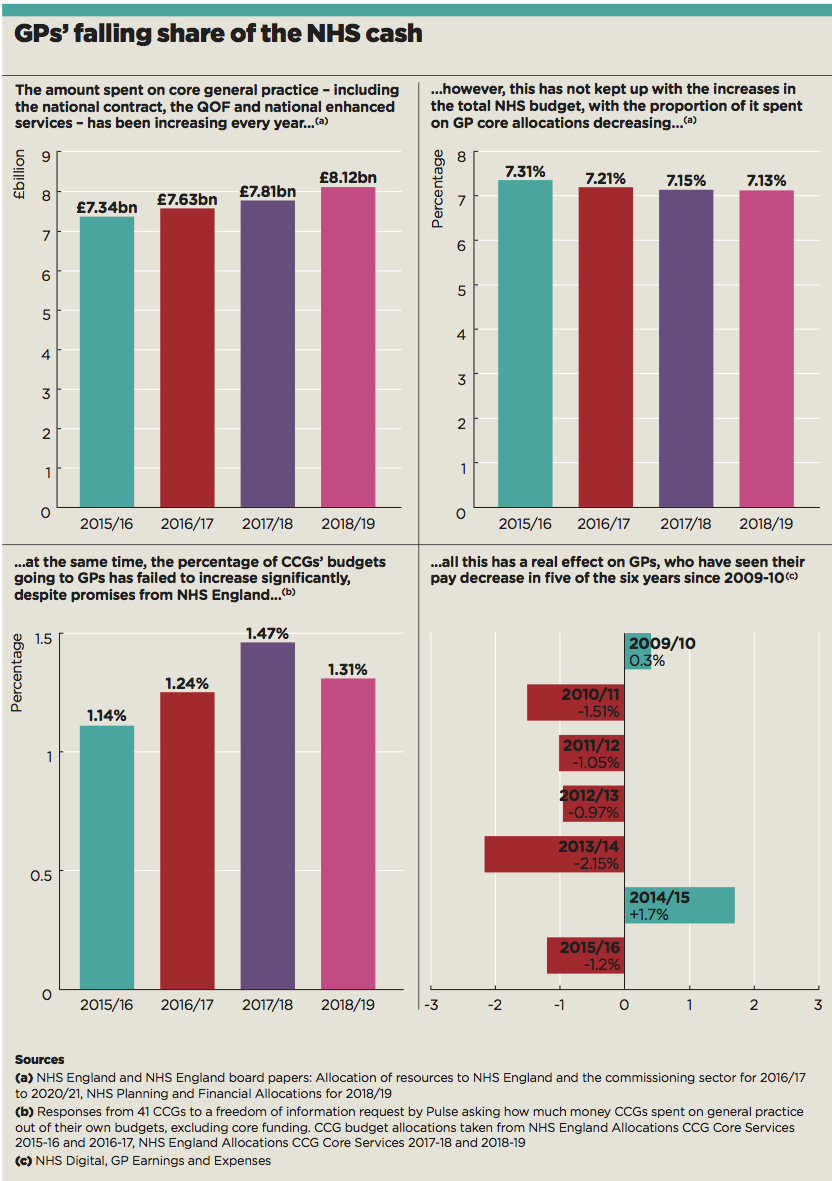
gp funding proportion
But RCGP chair Professor Helen Stokes-Lampard says the increase is ‘an important step forward to meeting our calls for our service to receive 11% of the overall NHS England budget… but it certainly doesn’t go all the way.’
For other GPs, the experience of years of disappointing plans and empty promises have left little hope that this latest announcement will change things for GPs on the ground.
London GP and GP Survival campaign group chair Dr Nicholas Grundy says: ‘The recent history of similar plans in primary care has been uninspiring and profoundly depressing.
‘If you look at the GP Forward View, on pretty much every marker it has failed. I don’t think there has been any material change in the general practice working environment and I think that’s because a lot of it has not been thought through.’
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens














