
David Cameron’s dream of GP practices opening all hours is fast becoming an expensive nightmare.
The first wave of his £400m ‘Challenge Fund’ pilots across England have tested seven-day access to GP practices and, in many cases, delivered questionable results.
Released with little fanfare last month, NHS England’s official evaluation of the first wave of seven-day GP access pilots made less than convincing reading.
It found a 15% reduction in minor, self-presenting A&E attendances after more than a year of the pilots. The £3.2m estimated savings in the pilot areas were significant, but were dwarfed by the schemes’ £50m initial funding.
The evaluation found that each appointment offered cost up to £50. It recommended that, given reported low utilisation on Sundays ‘in most locations, additional hours are most likely to be taken up if provided during the week or on Saturdays (particularly Saturday mornings)’.
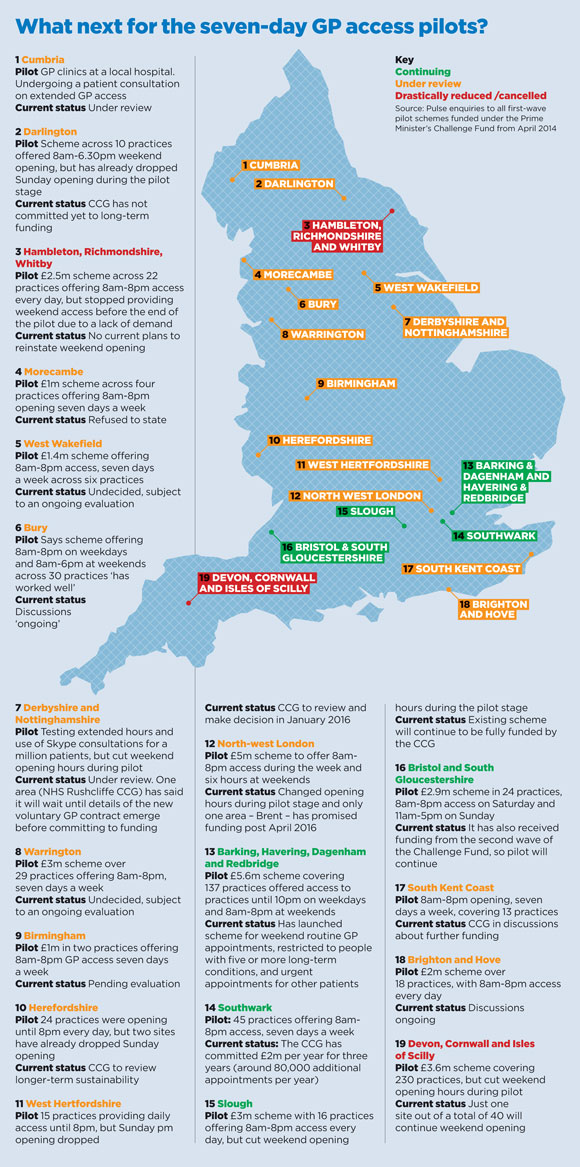
The Department of Health was quick to brand the first wave a ‘success’, but, as Pulse has reported before, the reality is that almost half of the pilots have already reduced their opening hours.
As central government funding runs out for the first wave, Pulse can now reveal that only two of the 19 areas providing seven-day access have fully committed to fund them beyond next March, while one has restricted access to patients with long-term conditions and another has had to apply for renewed government funding.
Two areas have told Pulse they intend to scale back their schemes. Devon, Cornwall and the Isles of Scilly has said it will not be funding the extended hours schemes beyond next April, other than a single site in Exeter that will provide a winter-only Saturday GP surgery service for 18 weeks from 7 November, 2016. NHS Hambleton, Richmondshire and Whitby CCG also said it had no current plans to reinstate weekend opening having dropped it earlier this year.
Uncertain future
Even enthusiastic areas, such as Bury – which has been held up by the Department of Health as evidence of the scheme’s success – are unclear about whether they will pursue the scheme. Despite a spokesperson saying the scheme has ‘worked very well’, discussions about its future are ‘ongoing’.
In summary, four of the schemes will continue in some form, two have drastically cut funding and 13 are reviewing their options. Unless additional money is found to allow CCGs to continue to fund the schemes, the likelihood is many will fall foul of cuts as commissioners try to balance their books.
NHS Southwark CCG is one area going ahead full-steam with seven-day GP access – but it is not cheap. The CCG has committed £2m a year for the next three years for 80,000 additional routine appointments from 8am to 8pm, seven days a week, at two sites in the south London borough.
NHS Slough CCG also told Pulse it is continuing to fund extra evening and weekend GP appointments, and commissioners in Barking, Havering and Dagenham, in east London, will continue to fund routine seven-day GP access, but it will be restricted to people with five or more long-term conditions. Bristol and South Gloucestershire will continue its scheme after receiving new funding from the second wave of the Challenge Fund.
Expensive luxury
GP leaders say the overall picture shows that seven-day GP access – even if managed through hubs, rather than requiring all practices to open every day – is an expensive luxury the NHS cannot afford at the moment.
GPC deputy chair Dr Richard Vautrey said: ‘At £43 a consultation, no reduction in hospital admissions and only minimal changes in A&E minor injury attendances, there must be real questions about the wisdom of continuing these schemes.’
The RCGP has written to the House of Commons Health Committee’s ongoing primary care inquiry saying it ‘rejects’ the seven-day GP access policy because it is ‘unrealistic due to the huge pressure general practice is under, with existing services in urgent need of resources’.
And Pulse has learned the pilots are causing real concern among out-of-hours providers. Chair of the Northern Doctors Urgent Care group John Harrison says the pilots are offering GPs up to double the out-of-hours rate – £100 an hour plus – meaning the group cannot compete.
He says: ‘We lost a quarter of our workforce within a couple of weeks. Not a lot of GPs want to do out of hours, so a scheme like this causes absolute mayhem.’
But the DH is under strict orders from Number 10 to make the scheme work. The first pledge in the Conservatives’ 2015 election manifesto said the party would ‘provide seven-day a week access to your GP and deliver a truly seven-day NHS’.
Although the scheme appears to be floundering, the Government is likely to find the resources to make it happen.
In July, Pulse learned the DH had raided £25m from the Primary Care Transformation Fund – previously the infrastructure fund designed to improve GP premises – to help fund the second wave of pilots, which launched this year.
Other areas are using NHS England’s ‘Vanguard’ pilot funding to carry forward seven-day access schemes. For example, the West Wakefield GP federation, a first-wave Challenge Fund pilot, is now trialling the ‘multispecialty community care’ model under NHS England guidance, which the federation said ‘encompasses evening and weekend services’.
The Treasury’s spending review (due to be announced tomorrow) could well assign some of the £8bn increase in NHS funding to extending seven-day working across the service.
The GPC may have ruled out agreeing to seven-day access requirements in the GP contract for next year, but negotiations are ongoing and it would be no surprise if the health secretary attempted to strongarm extended access in as a contractual requirement.
The wheels may be coming off, but don’t underestimate the PM’s determination to maintain momentum. GPs are in for a rocky ride.
What is the evidence?
- The Challenge Fund pilots found practices worked more ‘collectively’ and 90% of patients said extended GP opening hours was either very or fairly convenient1
- There was a 15% reduction in minor self-presenting A&E attendances in pilot areas, compared with a 7% reduction nationally. There was no discernible change in emergency admissions or use of out-of-hours services
- The average cost per appointment offered was typically in the range of £30 to £50
- Very low weekend utilisation figures (particularly on Sundays) contrasted with the ‘success’ of the weekday non-core slots
- The Department of Health said: ‘By 2020 this approach will be rolled out across the country as part of our plan for a seven-day NHS’
- But the GPC said the official evaluation raised ‘real questions’ about the wisdom of persisting with the schemes
- Another recent study found only 0.4% of people would benefit from Sunday GP appointments, with the majority preferring Saturday access.
References
1 NHS England. Prime Minister’s Challenge Fund: Improving Access to General Practice First Evaluation Report: October 2015
2 Simpson J et al. Access to general practice in England: time for a policy rethink. Br J Gen Pract 2015; 65:640;606 -607
References
2 Simpson J et al. Access to general practice in England: time for a policy rethink. Br J Gen Pract 2015; 65:640;606 -607
Reference
1 RCGP. The Future of GP Out-of-Hours Care. 2014.
*This article was updated at 12:10pm, 25 November 2015, to state on the map that Southwark CCG will provide over 80,000 extra appointments a year, and not 800,000, as it previously said.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens














