The humble face-to-face GP consultation may be in the process of becoming an anachronism.
Last month, NHS England revealed the first inklings of its new NHS app. It was confirmed that – among other things – the app will include built-in support for GP video consultations.
NHS England is not alone in being caught up in digital fervour. At south-east London superpractice the Hurley Group, ‘the volume of online consults doubled in the past year’, says Dr Murray Ellender, GP partner and co-founder of its online triage and consultation tool eConsult. The group’s long-term plan, he says, is to ‘only see the patients we need to see face-to-face, face-to-face.’
The Hurley Group – which has partners including former NHS England primary care director Dr Arvind Madan and former RCGP chair Professor Clare Gerada – now employs 12 GPs to work on eConsult. ‘Ideally, over the next six months, I’d like to double the size of that team,’ says Dr Ellender.
Dr Mobasher Butt, medical director at Babylon, which runs video consultation service GP at Hand with a west London NHS practice, estimates about ‘85% of cases can be dealt with entirely via virtual consultation’ – a figure he says is based on audits of ‘hundreds of thousands of patient records’.
The use of technology – whether it be video consultations or symptom-checkers (see box below) – to manage the number of face-to-face consultations has support across the board, from the BMA and RCGP to the UK’s four governments. Crucially, it is the second of new health secretary Matt Hancock’s stated priorities, after ‘workforce’.
How the new technology works
Online assessments
How do they work? Patients fill in an online questionnaire about their condition or symptoms, which is sent to a GP, who assesses the information and responds.
Which companies are using them? One of the best-known providers is eConsult, developed by the Hurley Group NHS superpractice in London. It is currently used in 400 NHS practices in 46 CCGs and is available to 4.2 million patients.
Symptom-checkers
How do they work? Patients answer a series of questions through an app or website about their symptoms, and are then given automated on-screen advice about what clinical services are most appropriate.
Which companies are using them? Many providers offer a symptom-checker but private firm Babylon, which also provides the GP at Hand NHS service, has made the bold claim that its version can offer advice ‘on par’ with that of GPs, thanks to the artificial intelligence behind the technology – a claim disputed by the RCGP.
Video consultations
How do they work? Patients book a video appointment via an app or computer and choose a time slot and GP that is convenient for them. GPs then carry out a video call in which they assess the patient remotely.
Which companies are using them? Push Doctor was one of the first to offer video consultations. At launch in 2015, its fee-paying service had a network of more than 7,000 GPs.
Yet some experts are urging caution, citing a lack of evidence and safety implications for patients. There are also fears that online consultations could harm efforts to tackle antimicrobial resistance, and even doubts that the technology will reduce GP workload.
Despite such warnings, there is little doubt technology is set to play a much bigger part in GPs’ lives, most obviously through the NHS app.
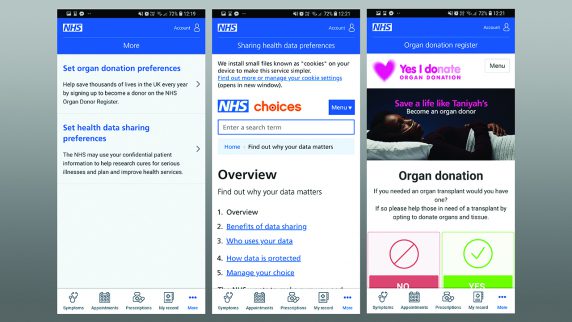
Before standing down as health secretary, Jeremy Hunt said the NHS app would allow users to book GP appointments, check symptoms, receive triage advice, access medical records, order repeat prescriptions, change data sharing and organ donor preferences and promote ‘approved apps’.
The Gizmodo website obtained further details on the testing of the app, revealing it would take place in 10 practices this month. In its initial stages, it will allow patients to specify preferences for ‘end of life’ care, which will be passed to their GP.
NHS England’s aims include enabling the app to connect with other devices, such as Apple Watch or Fitbit, share data and, crucially, enable video consultations.
NHS England is serious about this. It committed £45m over three years to help practices implement technology. Practices must put this funding towards systems that allow patients to send a query or symptoms to their GP – and potentially video consultations. A total of 39 CCGs were given funding in 2017/18 to implement new technology.
Safety concerns over remote consultations
However, caution is warranted. When the CQC inspected 35 online providers in 2016/17 it found 43% were not providing ‘safe’ care. Inspectors pointed to high volumes of opioid-based medicines being prescribed without talking to the patient’s registered GP, and inappropriate prescribing for long-term conditions
The CQC report also highlighted inappropriate prescribing of antibiotics – ‘a particular challenge for video-based services’. It cited ‘examples where, because the clinician was not able to effectively carry out the usual clinical assessment… such as examining a patient’s chest, ears or throat, the threshold for prescribing antibiotics had been lowered.’
‘You can’t do a proper physical examination online,’ insists Dr Jackie Applebee, east London GP and deputy chair of Doctors in Unite. ‘If we’re just taking a history and it’s something fairly minor and self-limiting then it’s what we do on the phone. But as soon as we do a physical examination, that’s different.
‘And that’s not just getting our stethoscopes out or putting our hands on somebody’s abdomen, but observing somebody’s demeanour – whether they’re out of breath when they walk down the corridor. We make those assessments subconsciously – and all of that will be lost online,’ Dr Applebee adds.
Claims of symptom checker advice being ‘on par’ with GPs
Fresh concerns are now centring on artificial intelligence. GP at Hand gives patients advice about symptoms through an interactive symptom-checker that asks questions about their condition.
Babylon claimed in June that the advice was ‘on a par’ with that of GPs, as it had achieved similar scores in GP exams as an average trainee.
This caused a backlash. The firm had used the RCGP’s trainee exams in its testing, prompting college vice-chair Professor Martin Marshall to comment: ‘To say Babylon’s algorithm has performed better than the average MRCGP candidate is dubious. No app or algorithm will be able to do what a GP does.
‘There are many factors to take into account, a great deal of risk to manage, and the emotional impact a diagnosis might have on a patient to consider,’ he said at the time.
Research suggests symptom-checkers cannot always be relied on.
A US study published in the BMJ in 2015 analysed 23 symptom-checkers and found the correct diagnosis was provided in 34% of cases and appropriate triage advice given in 57% of instances. It found the symptom-checker on NHS Choices correctly triaged emergency and urgent conditions in 87% of cases – but also incorrectly triaged non-emergency or non-urgent conditions in 80% of cases.
There is an even more fundamental point here. These symptom-checkers do not reflect the reality of the diagnostic process.
As the King’s Fund put it in 2010: ‘In theory, on seeing a patient presenting with a set of signs and symptoms, a GP may follow a simple, linear sequence from history-taking and examination through to a differential and then final diagnosis. However, the reality of the diagnostic process is often quite different.’ Research has shown that only 30% of face-to-face consultations end with a diagnosis.
Yet these symptom-checkers use this linear sequence – patients input their symptoms and then receive advice. Hertfordshire GP and deputy chair of UK Conference of LMCs Dr Katie Bramall-Stainer said: ‘Patients don’t present in nice neat compartmentalised boxes – so the technology will need to be more nuanced.
‘I am not yet aware of robust evidence showing how these platforms materially and safely manage demand and what potential indemnity issues could arise from incorrect diagnoses.’
Indemnity fees ‘reflect higher risk’
The medical defence organisations seem to agree on risks to patient safety. The MDU says its fees for GPs ‘reflect the higher risk’ of providing online services. This is ‘because of the limitations it can impose – for example, whether doctors are in a position to make an appropriate assessment of the patient’s symptoms’.
MDDUS medical division joint head Dr Anthea Martin points to ‘inherent risks’ of online consultations, such as ‘lack of prior knowledge of a patient, ensuring adequate consent and providing continuity of care’.
And there are even doubts around another key selling point of technology – that it will reduce GP workload.
A Society for Academic Primary Care study of 36 practices using eConsult found ‘unless use of online platforms increases and integration with IT systems improves, online consultation systems are not likely to have any notable impact on patient waiting times and staff workload and may add to practice workload’. More than a third of online consultations also required a face-to-face consultation, it found.
But with the NHS and the new health secretary fully supportive of increased technology, such concerns look unlikely to stop the march away from traditional face-to-face consultations.
The NHS app: what it will involve
The new app is to be tested in 10 practices towards the end of this month. Initially, it will allow users to:
- Make GP appointments
- Order repeat prescriptions
- Manage long-term conditions
- Access 111 online for urgent medical queries
- State preferences for data-sharing, organ donation and end-of-life care
There are further plans for the app to:
- Enable GP video consultations
- Link to other apps, such as Fitbit and Apple Watch
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens