With GP trainee numbers up, why is Hunt rolling back his 5,000 target?

Last month, it was announced that a record number of GP trainees had been recruited to start this year in England.
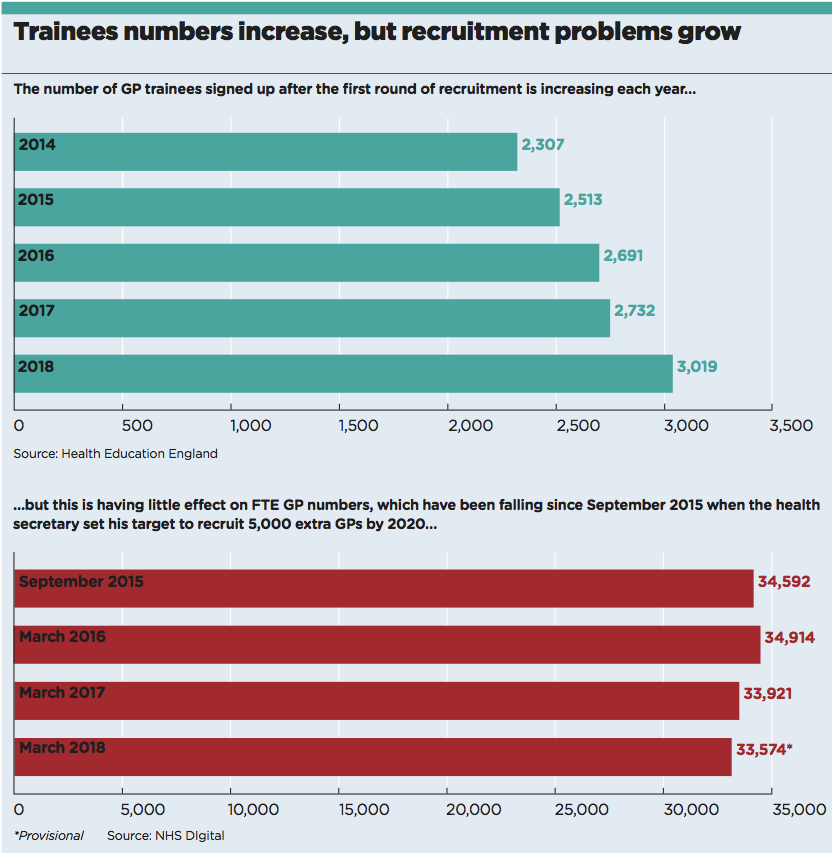
It seems that, for the first time, health managers will be successful in meeting their target to recruit 3,250 GP trainees in a single year. Although the target was first set almost three years ago, this should still be a cause for celebration, especially as it means half of all medical graduates will enter general practice.
And yet… the news followed hot on the heels of health secretary Jeremy Hunt telling the Guardian he was ‘struggling to deliver’ on his target to recruit 5,000 extra GPs in England by 2020.
A Pulse survey has also revealed that this struggle is having a real effect on practices – 15% of all GP positions are currently vacant, a significant jump from the 12% seen in 2016 and 2017.
It seems likely Mr Hunt made his admission because he could no longer claim otherwise. Since he set the goal in September 2015, England has actually lost more than 1,000 full-time-equivalent GPs – putting him 6,000 adrift of the 5,000 target.
However, his acknowledgement is still significant. He told the Guardian: ‘We do need 5,000 more GPs and we are struggling to deliver that pledge, but I’m absolutely determined to do so because GPs are working incredibly hard; too hard.
‘I got quite widely ridiculed when I made the pledge in 2015. I wanted to nail my colours to the mast of getting more GPs into the system. But it has been harder than we thought.
‘This is not a pledge we’re abandoning because it’s a very, very important pledge for the NHS and with general practice. It’s just taking a bit longer than I had hoped.’
In other words: we’re not abandoning the pledge, but don’t expect us to fulfil it.
recruitment issues
But how can GP recruitment be struggling when medical graduates are signing up to the profession at a greater rate than ever before?
Health Education England chief executive Professor Ian Cumming suggested it was due to newly qualified GPs leaving the profession. He told last month’s NHS Confederation conference in Manchester that just 60% of GPs who gained their completion of training certificate in general practice five years ago are in ‘substantive or long-term locum appointments in this country’.
He added ominously: ‘As every year goes by, beyond five years, that number [of GPs working outside full-time roles] goes up slightly. We have to address it.’
But although this 40% cohort of GPs who are not in full-time roles contributes to the lower official FTE numbers, this may not be as damaging to the profession or the NHS as it sounds.
As Professor Cumming went on to add, those 40% are ‘doing short-term locums, they are doing other things now’.
But are short-term locum roles – or ‘other things’ – necessarily a bad thing? As Pulse’s special issue on trainees last August revealed, younger GPs are more likely to want portfolio careers, spending some time locuming or in a part-time salaried role.
Indeed, of the 40% of respondents who told Pulse they eventually want to be GP partners, half said this would be in combination with roles in academia, military, CCGs or occupational health – all of which benefit the NHS.
Dr Angela Goyal, a portfolio GP and founder of Inspired Medics, which recently ran an event on portfolio careers, said: ‘Portfolio careers are a great way to retain GPs. You are also providing useful skills. We need GPs who have secondary interests.’
She added that GPs look to do more locum work so they can ‘see general practice in different settings’.
So does this mean we can relax about the fall in GP FTEs? Sadly not. A Pulse survey of 660 GPs on vacancy rates reveals around one in six GP positions is unfilled – the highest since Pulse started collecting the data. But it seems the problems come later down the line – in retaining older GPs in full-time practice.
More than four in 10 respondents to last year’s BMA survey of 2,000 sessional GPs had previously been a GP partner, while two-thirds stated they had reduced their hours and changed their working pattern. The average age of sessional GPs was 44 for females and 49 for males.
Meanwhile, this year, Pulse revealed that the average age of GPs drawing their pensions for the first time fell from 60.4 years in 2011/12 to 58.5 years in 2016/17.
The NHS does run a retention scheme that incentivises GPs considering retirement to continue working up to four sessions a week. Their practices also receive funding.
But Dr Krishna Kasaraneni, an executive member of the BMA GP Committee, said the retention scheme can only do so much and keeping older GPs in the profession ‘needs significant work’.
He said the more fundamental issue is ‘managing workload and increasing funding to keep GPs in the system’.
Which will require a political will that we have seen scant evidence of for quite some time.
The decline and fall of the 5,000 GP pledge
May 2012 – Then health secretary Andrew Lansley announces a target for 3,250 of medical graduates to enter general practice every year – 50% of all medical graduates.
October 2014 – Health secretary Jeremy Hunt first makes the pledge for 5,000 extra GPs by 2020 at the Conservative Party Conference, saying England would be self-sufficient in terms of training GPs.
March 2016 – Health minister Lord Prior tells Parliament ‘there is a risk whether we will be able to get that number into general practice’.
April 2016 – NHS England’s GP Forward View announces a ‘major recruitment campaign’, including £20k bursaries, a retention scheme to keep GPs in the profession and a programme to recruit GPs from overseas.
May 2017 – NHS Digital figures reveal the number of full-time-equivalent GPs decreased by 221 between September 2015 – the baseline for the 5,000 extra GPs target – and March 2017, meaning the Government needs to increase the workforce by 5,221.
July 2017 – NHS England chief executive Simon Stevens announces that the overseas recruitment scheme is to be quadrupled to an ‘industrial scale’, with an aim to recruit 2,000 GPs from overseas, up from the 500 specified in the GP Forward View – concluding this is necessary to meet the target.
May 2018 – Official figures reveal the workforce is 1,018 GPs worse off than it was in September 2015.
June 2018 – Mr Hunt concedes that he is ‘struggling to recruit’ the 5,000 additional GPs – but insists the target remains in place.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens










