The health secretary has spoken proudly about the ‘extra £250m put in to the GP contract’ this year, in the form of funding worth £5 per patient for practices to support care of vulnerable elderly patients.
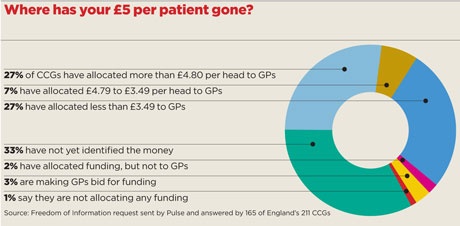
But a Pulse investigation reveals that a third of areas have yet to allocate any of this funding.
A request by Pulse under the Freedom of Information Act, answered by 165 CCGs, has found only £97m of the money meant to support patients identified under the unplanned admissions DES has been spent on GP services.
When extrapolated across the country, this figure equates to around £124m – barely half the funding health secretary Jeremy Hunt claims has been given to support practices.
In fact, only a quarter (27%) of CCGs have actually spent all the funding on GP services. Instead, some have used it to plug gaps in secondary care funding.
Even where CCGs have committed money to GP services, it has been linked to additional targets or been repackaging of existing funding.
There was no guarantee from NHS England that the funding would have to be spent on GP practices – but there were heavy hints.
In guidance for CCGs, released in December 2013, NHS England said: ‘CCGs… will be expected to provide additional funding to commission additional services which practices, individually or collectively, have identified will further support the accountable GP in improving quality of care for older people.’ It added: ‘This funding should be at around £5 per head of population for each practice.’
NHS England deputy chief executive Dame Barbara Hakin said this was ‘concrete’ guidance that funding should be transferred from the hospital-based budget and the health secretary hailed this move in the Government’s Transforming Primary Care policy document.
CCGs struggling
But the strategy was always dependent on CCGs finding the money themselves, and the shortfall GPs have seen reflects the perilous state of CCG finances.
Overall, a staggering one in three CCGs has so far failed to identify the money – halfway into the first year of the DES and ‘named GP’ policy.
In two CCGs – NHS Mid-Essex and NHS South Gloucestershire – there is simply no money in the pot.
NHS Mid-Essex CCG is forecasting a 2014/15 in-year deficit of £15.8m and a year-end cumulative deficit of £24.9m, and has been declared to be in ‘financial recovery mode’ by NHS England.
NHS South Gloucestershire CCG says it is unable to devote the funding because of its deficit, which NHS England is aware of. A spokesperson says: ‘The CCG’s financial position was approved by NHS England as part of our two-year operational plan and five-year strategic plan.’
This highlights a major problem for CCGs – that they are having to deliver the health secretary’s promise without any extra funding, while ensuring all parts of the health service continue to work.
Dr Steve Kell, chair of NHS Bassetlaw CCG and co-chair of NHS Clinical Commissioners, says: ‘It isn’t as straightforward as doing this in one year. I think that is where CCGs struggle, without some transformation funding.’
In some areas, the money is being used to plug gaps in other areas of the local health economy.
Plugging gaps
NHS Coventry and Rugby CCG says its A&E attendances have increased by 8% since last year and, as a result, it will have to use the money to support the acute provider.
A spokesperson says: ‘We are confident that the £5 per head spending plans that we are developing with our member GPs will, once fully implemented, help address these emergency pressures. In the meantime, we are inevitably having to utilise the investment slippage to reimburse our acute provider for the additional work that is being undertaken.’
And even in areas where the money has been allocated to practices, there are strings attached.
NHS Stockport CCG, for example, has asked practices to submit bids to earn up to £6 per head of population in extra funding in return for extended hours, better urgent care in-hours, better long-term condition management and more proactive management of care home patients.
Similarly, NHS Erewash CCG has allocated £300,000 – equating to £3 per patient – to a nursing home scheme, which practices can bid to take part in.
And, as Pulse has previously reported, there are schemes that link the funding to hard admissions targets.
Practices in NHS Ipswich and East Suffolk CCG are getting an additional investment of £2.45 per patient to help them reduce unplanned hospital admissions for patients over 75.
But if a practice is successful in hitting targets for reducing admissions among elderly patients, it will be rewarded by a further £2.45 per patient, making £4.90 in total.
NHS Halton CCG has also tied full payment to outcomes, holding back 50p per patient from practices, which will be paid depending on hitting a target of reducing admissions for over-75s by 2.5%. Sixteen practices will be sharing £600,000 if they hit these targets, equating to £4.65 per patient across the whole population.
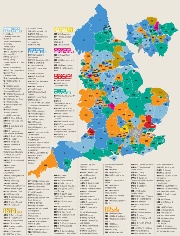
Map: Has your CCG given £5 per patient?
But this has not stopped the health secretary extolling the £5 per patient as an important shift of resources to support older people.
Last month, Mr Hunt told Pulse GPs were ‘central’ to the Government’s health strategy, citing the example of the ‘extra £250m that we put into the GP contract last year to improve care for the most vulnerable older people’.
He gave a similar message to the RCGP conference. He told delegates: ‘Last year we had the extra £250m, the £5 a head that came alongside the GP contract. When you add that to the £150m that was freed up in the DES, there is £400m we have made available to help boost proactive care for the most vulnerable older people.’
But GP leaders say the additional resources are not being given to all practices, even though they are essential if GPs are to do what Mr Hunt would like them to. GPC chair Dr Chaand Nagpaul says: ‘I believe all practices should have received the £5 per head because it is just not possible to look after older people in the community on the back of an enhanced service. It always required that additional resource.’
What money should practices be expecting?
What was promised exactly?
In December 2013, NHS England announced plans in its ‘Everyone Counts’ guidance for CCGs to ‘support practices in transforming the care of patients aged 75 or older and reducing avoidable admissions by providing funding for practice plans to do so’. This was set at £5 per head of population.
Were practices supposed to receive it?
Not necessarily. The guidance said the funding was for ‘additional services which practices, individually or collectively, have identified will further support the accountable GP in improving quality of care for older people’. However, since then, the health secretary has repeatedly used this to suggest he has given money directly to support practices.
When was it supposed to be available?
The funding was intended to support the ‘specific focus during 2014/15 on those patients aged 75 and over and those with complex needs’ under the ‘named GP’ scheme and unplanned admissions DES. However, no timescale was set. Some CCGs are still formulating their plans (see map, page 10) so practices may yet receive funding.
Is it recurrent?
NHS England made no promise. However, the guidance did say: ‘Practices should have the confidence that, where these initial investment plans successfully reduce emergency admissions, it will be possible to maintain and potentially increase this investment on a recurrent basis.’
What other funding was available?
Jeremy Hunt has referred to £400m for practices: the £250m for the £5 per patient, and £150m for the unplanned admissions DES, although this was money recycled from the QOF.
Disappointment
Official guidance from NHS England recommended CCGs should give practices ‘confidence’ the funding could be made recurrent. But there is little sign of this happening. Dr Mark Sanford-Wood, interim secretary of Devon LMC, sums up GPs’ thoughts: ‘Overall, the feeling on the ground is one of disappointment.’
NHS North, East and West Devon CCG has ring-fenced £1.25m for practices to develop plans to support older patients, equating to £1.25 per patient, and even then, the LMC says GPs haven’t seen the money yet. The CCG says it might invest more in future, but only after assessing the results of the first tranche of investment.
But Dr Sanford-Wood says: ‘The official line is that if the £1.25 goes well, another tranche might be available. However, even CCG managers appear highly sceptical about any further money and I know of no GPs who believe we will receive more than the initial amount.’
When approached by Pulse to explain, a DH spokesperson simply said: ‘CCGs are not restricted to using this funding on general practice – in some areas, CCGs have used it to employ extra district nurses for local practices.’
Dr Peter Swinyard, chair of the Family Doctor Association, says he is ‘not even remotely’ surprised that GPs are not receiving the promised funding.
He says: ‘I haven’t seen any string-free money coming out of NHS England ever, or from the Department of Health before them for a very long time.
‘I think the money should perhaps have been more carefully badged to show it actually should be paid to practices, perhaps in return for something or other. But mostly it has been hijacked for other purposes.’
Dr Grant Ingrams: ‘Unexpected A&E activity means our £5 per head has been raided’

My understanding was that this money was supposed to go to general practice for providing care for over-75s.
But in our case, the CCG has said ‘we are going to spend the money elsewhere therefore don’t even bother putting in your applications’.
The CCG has had unexpected activity within the A&E department at our local hospital and they therefore told us that there was less money available for the £5 per head of population.
The CCG has opted not to invest in care for vulnerable elderly patients in general practice, which can lead to increased pressure on the hospital in future. To say that we are going to take that money out, which may have actually started to turn that tide of patients going into hospital, in order to shore up secondary care is, to my mind, very shortsighted.
The worrying, sad thing is that local GPs are just not surprised that the money, despite being part of a national initiative, is being taken away to be put into secondary care again.
Although GPs are really angry – there was an open meeting held where there were quite palpable feelings of anger – they are really just wondering what on earth is going on, when the CCG is taking money from general practice to put into hospital, which is really the reverse of what they were designed to do.
We know there is nothing to be gained from raising this issue with the CCG again for this year. There is no point, the money is taken. But I think that the CCG has been given a strong message from its membership that we don’t expect to see such things again, so I hope it will listen. It is supposedly a membership organisation.
Dr Grant Ingrams is a GP in Coventry, and a member of the GPC
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens