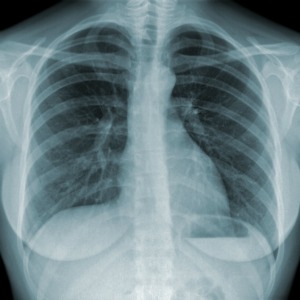
Tuberculosis rates in England are at their lowest levels since 1990, Public Health England has said.
The number of patients with TB has fallen by 38% since 2011, with experts hopeful that the disease could soon be eradicated.
Figures from the Tuberculosis in England: 2018 report show that TB levels hit a peak in England in 2011, with 15.6 cases per 100,000 population, but dropped to 9.2 cases per 100,000 in 2017 – below World Health Organisation-defined figures for low incidence.
PHE noted that the number of latent TB infection (LTBI) tests carried out on recent migrants to England increased by 73% between 2016 and 2017, and recommend in the report that GPs keep inviting new migrants for LTBI testing in high-burden TB areas.
In 2016, NICE called for commissioners to consider financial incentives for practices for identifying and screening high-risk patients.
PHE also noted that there is still a delay between symptoms appearing and diagnosis for many patients and suggested that there needs to be more TB education among staff in general practice to reduce diagnostic delay.
Dr Sarah Anderson, head of TB strategy at PHE, said: ‘It is hugely encouraging to see a continued decline in TB in England which shows that the interventions we are putting in place are having an impact and will hopefully one day soon consign TB to the history books.’
But she added: ‘While these new figures are positive, challenges still exist. The proportion of people who experience a delay between symptom onset and diagnosis remains stubbornly high.
‘We are working across England to ensure that patients are diagnosed and treated as soon as possible to minimise the chance of long-term ill health and onward transmission.’
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens