Investigation: Are we at risk of running out of GPs?
Frinton-on-Sea finds itself at the sharp end of the GP recruitment crisis. According to LMC leaders, the Essex seaside town is experiencing such a dearth of full-time GPs that there is currently just one serving more than 8,000 patients.
The crisis has become so great in north-east Essex that NHS England managers have had to step in to ‘immediately address’ the situation and support practices.
Essex LMCs chief executive Dr Brian Balmer even warns that the future of traditional general practice is at stake.
He says: ‘That area is struggling because several practices are very short on doctors, but they’re not alone. Normal-type general practice is simply going to disappear in some areas.’
Recruitment problems are not confined to Essex. A Pulse investigation suggests some 149 practices in England have more than 4,000 patients for each full-time-equivalent (FTE) GP. Ministers, experts and GP leaders are in rare agreement that the country needs more GPs, even if they are divided over how many.
The RCGP estimates that an additional 10,000 GPs need to be recruited and trained in order to accommodate the workload shift from secondary care, the growing burden of demand from an ageing population and the demands of seven-day opening. The college has based its estimate on roughly one additional GP being needed in every practice across the UK.
The Centre for Workforce Intelligence (CfWI) says its projections show that for deaneries to meet their target for GP registrars to make up 50% of specialty training places from 2015, a yearly intake of 3,250 GP trainees will be needed. If this goal is met, the CfWI predicts there will be an additional 12,800 FTE GPs by 2030, bringing the total workforce up to around 83-84 GPs per 100,000 population.
Ministers have officially adopted the 3,250 GP trainee target, but even these estimates may not go far enough, according to health secretary Jeremy Hunt.
In a speech last year, Mr Hunt said the additional responsibilities he expected GPs to take on were likely to mean more were needed. ‘It may be that we need to increase those numbers still further,’ he said.
Pulse has obtained figures that show a wide disparity in GP numbers across the UK. A Pulse analysis of 2012 data from 8,088 GP practices in England, collected by the Health and Social Care Information Centre, shows that – excluding locum support – 149 practices had more than 4,000 patients per FTE GP and 75 were coping with more than 5,000 per GP.
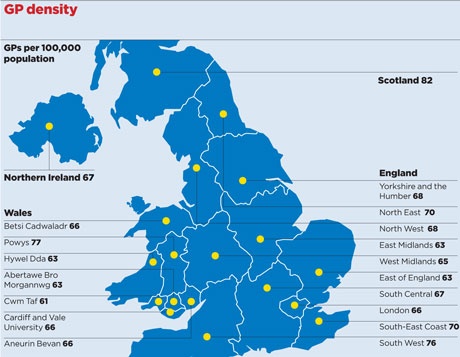
There were 67 GPs per 100,000 patients in England in 2012, but this ratio varied considerably, with a continuing trend for more deprived areas to have fewer doctors (see map, above).
Northern Ireland and Wales had similar overall GP densities in 2012, at 67 and 66 GPs per 100,000 patients respectively. Data for Scotland showed a more favourable picture, with around 82 GPs per 100,000.
Progress on recruiting more GPs has so far been slow. While there was a significant hike in the proportion of trainees going into general practice last year, up from 36% to 41%, this increase was largely down to a sudden drop in specialty training posts.
The actual increase in GP trainee places was just 95 compared with the previous year. The total number recruited – 2,725 – fell far short of the 3,250 needed next year and beyond.
Pulse has learned that Health Education England has commissioned a GP taskforce, led by Dr Simon Plint, postgraduate dean at Wessex Deanery, to develop a more coherent recruitment and retention strategy.
The taskforce is in the process of finalising a report calling for better marketing of general practice as a career to medical students, increased training capacity and capping recruitment into other specialties – as well as devising strategies to improve the retention of existing GPs.
Professor Bill Irish, director of GP education at Health Education South West and chair of the Committee of General Practice Education Directors, says: ‘There are good numbers applying in Northern Ireland, London and the South of England, but a relative paucity of good-quality applicants in the north of England. This is a bit of a “double-whammy” as these tend to be the areas with high healthcare needs.
‘Why that is is difficult to say. But it probably relates to the aspirations of doctors around quality of life and workload, which drives them to the home counties, south coast and similar areas.’
In the meantime, GP leaders are working on various possible solutions to what appears to be an ongoing crisis. Whether any of these will help reverse the trend remains to be seen.
How many more GPs do we need?
10,000 more GPs needed to staff seven-day working: RCGP
12,800 extra full-time-equivalent GPs needed by 2030: Centre for Workforce Intelligence (CfWI)
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens