This fearmongering over missed cancers will end up costing us GPs
There are many aspects of the job that cause me anxiety, but I tend to worry most about missing a diagnosis of cancer. As a perfectionist, I hate getting anything wrong, especially a diagnosis as important as cancer.
I should probably accept that I will get it wrong sometimes, and when I do it will inevitably lead to a misdiagnosis, a delayed diagnosis and even the death of a patient. It doesn’t sit comfortably with me and I can think of at least two patients that I have seen in the last few years that have had a diagnosis of cancer missed by me.
So perhaps I am being understandably touchy when I get annoyed by the mainstream press reporting that two-thirds of cancer diagnoses are missed by GPs. Behind the headline, I suppose what this means is that only a third of bowel and lung cancer diagnoses are made via the ‘two-week wait’ pathway for suspected cancers.
Now patients may simply not see a GP before a diagnosis, cancers may be diagnosed incidentally on imaging arranged for another reason. Patients may be so sick that they need admission to hospital. Patients may become unwell between the time of referral for investigation and the date of their outpatient appointment.
We can miss the cancer needle in the growing haystack of patient demand
But it’s also worth remembering that patients and their symptoms don’t always follow the textbook. Vague symptoms, atypical symptoms, absence of symptoms and diagnostic overshadowing can all mean that we can miss the cancer needle in the growing haystack of patient demand. One could also argue that growing GP workload means that we are prone to decision fatigue and therefore more likely to miss diagnoses and misdiagnose.
The alternative to acting as the prudent gatekeepers of the NHS and being its risk sink is to simply refer more. Refer anybody with vague symptoms, a slight change in their bowel habits or a bit of bloating after a curry. This will both overload secondary care, who struggle just as much as general practice with workload and workforce issues, and have a massive psychological impact and knock-on effect on our patients.
What rips my knitting the most, though, is the impact that the spinning of such ‘research’ has on morale. I have no doubt that it makes already hard-pressed GPs wonder why they bother. It may well be the final nail in the career of a young or experienced GP. But bad news and fearmongering sells papers and generates clicks.
The conspiracy theorist in me can’t help but wonder who would bring the attention of the mass media to an article in a low-impact Dutch epidemiology journal. Either it’s the publicity-seeking cancer charities who funded it, or it’s Richmond House exerting yet more leverage over a beleaguered profession.
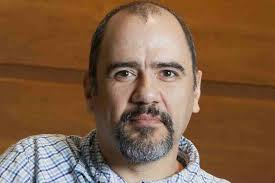
Dr Samir Dawlatly is a GP partner in Birmingham
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.










