Revealed: The rising tide of GP burnout as NHS cuts support
Exclusive Rising numbers of GPs are so stressed during their working day that they are at a high risk of burning out completely, reveals the largest ever survey conducted in the profession.
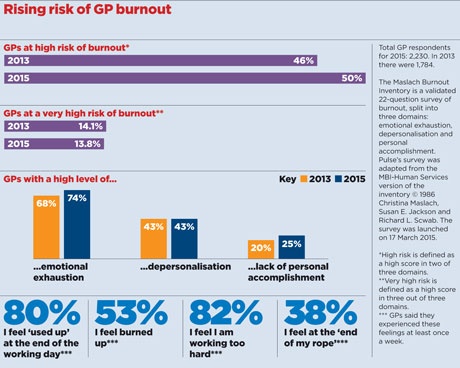
The Pulse survey of 2,230 UK GPs shows 50% are at high risk of burnout, up four percentage points from the same survey two years ago.
GP leaders say the health service has become an ‘industrial hazard’ and that burnout is forcing more GPs to leave the profession.
But the few occupational health schemes providing support to struggling GPs in England have had their funding cut and in Scotland NHS managers are looking at charging for their services.
The Pulse survey shows that three-quarters of GPs feel emotionally exhausted while 25% report a low sense of personal accomplishment.
Dr Daniel Mounce, a former GP in Bradford, left the profession ‘after falling apart mid-consultation’.
He said: ‘For me, leaving general practice has been like leaving an abusive relationship. The shaming and invective, the fear, the unreasonable demands were about driving down self-esteem. I can’t quite believe I ever thought I could stick it for another 30 years.’
Doncaster GP Dr Shahzad Arif, who was recently slapped with a breach notice by NHS managers after burnout forced him take sick leave, told Pulse he was ‘frustrated’ at the total absence of support.
He said: ‘I think it was perhaps something waiting to happen; there was a slight trigger that day because the practice had been unusually busy and I decided I need a break, I couldn’t go on.’
In response to the first burnout survey, Pulse launched its Battling Burnout campaign that last year won a pledge to fund occupational health support for all GPs in England.
But NHS England has yet to release the long-overdue service specifications, and in the meantime has slashed funding for previously excellent mental health support services in Devon, leaving GPs to resort to self-funding.
In Lancashire and Cumbria, LMC chief executive Peter Higgins said that NHS England scrapped the previously ‘very good’ services in 2013, and it has so far refused bids from the LMC to have mental health service put in place.
In Kent, LMC medical secretary Dr John Allingham said: ‘We are hanging on by the skin of our teeth. We have occupational health funding for next year, but nothing guaranteed going forwards.’
It is the same case in Lothian, where GPC executive member Dr Dean Marshall tells Pulse there was a counselling service and occupational health ‘but now they’re talking about charging GPs for it’.
Former RCGP chair Professor Clare Gerada, medical director of a confidential mental health service for doctors in London – said: ‘The NHS at the moment is an industrial hazard, and especially for GPs. Of course we go beyond the call of duty, but to do so every single day is causing great harm to GPs.’
Professor Gerada said her service – the Practitioner Health Programme – had been forced to shut its doors for six weeks in March after a ‘massive increase’ in demand, most of it from GPs.
It comes as the Government plans to roll out seven-day working for GP practices and NHS England’s Five Year Forward view plans for GPs to take on more care outside hospitals. The health secretary promised GPs a ‘new deal’ that will be announced this month to ‘look at why GPs have so much burnout’.
GP survival skills
Ten coping strategies for the worn-out GP
How I found a way to survive in general practice
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens










