Outlook bleak as trainee applications hit new low

‘I have seen the GP career go from one that was quite attractive to something that is very unpopular,’ says Anish Koneru, a medical student at Imperial College London.
Having once had an ‘open mind’ about a career in general practice, he has now ruled it out for good.
And he is not alone.
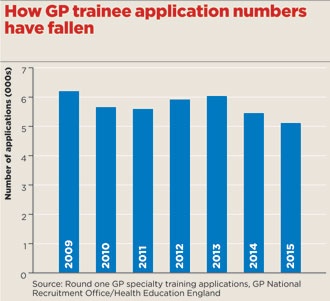
The number of medical graduates applying for general practice across the UK has gone down by 6% this year, hitting a six-year low.
Yet this comes at a time when the NHS, the Department of Health, the BMA and the major political parties all agree that boosting GP numbers is essential for the long-term future of the NHS.
As a further kick in the teeth to practices struggling to recruit, the figures come just a month after NHS England laid out its plans to boost the number of new GPs working for the NHS.
Health Education England is refusing to provide a regional breakdown of these figures, which include Scotland, Wales, Northern Ireland and the Defence Deanery. But Pulse understands there are substantial regional variations.
HEE claims that, in England, it is ‘well on course’ to meet its target of 3,250 new GP trainees a year.
But GP leaders believe it may be too late to avert a looming shortage of GPs, despite fevered efforts behind the scenes to do so.
Worrying prospects
The national figures for applications, obtained by Pulse, show a fall of 6.2% on last year, with only 5,112 applicants in total.
This is an 18% drop compared with the 2009 high of 6,200 applicants – the first year for which figures are available.
The figures paint a disturbing picture of the prospects for the profession.
A Pulse analysis of previous years’ figures shows that, on average, 54% of applications result in filled positions. This year, that would translate into just 2,760 positions across the whole of the UK being filled by the summer – far short of the 3,125 training positions available in England alone this year.
In HEE’s East of England region, the situation is ‘dire’, according to Dr Tim Morton, chair of Norfolk and Waveney LMC, where there were just 336 applications for 332 places this year. Traditionally, there are 1.7 applications per post in the region, meaning educators were expecting more than 560 applications this year.
Dr Morton says: ‘The profession’s warning cries have been ignored, and now they are coming true. The huge concern is that we have over-50s retiring early, partly because of the intolerable workload, and practices find themselves in a position where they cannot recruit because there are not enough younger doctors coming through the training schemes.’
And he warns that the situation in the East of England is not unusual.
‘This is national. I talk to fellow LMC chairs across the country and this is the norm, not the exception. [But] we’re in a better position than Wales, West Midlands and Yorkshire, which I find quite frightening.’
The LMC is working with HEE and NHS England to try to solve the crisis. ‘But this is about five years too late’, Dr Morton says.
It looks as though a repeat of last year’s training turmoil is on the cards. HEE was forced to introduce an unprecedented third round of recruitment last July, after some areas saw 40% of posts unfilled after the second round.
The health education body even had to introduce a ‘pre-GP training year’ in hospitals for applicants who failed to pass the assessment processes, which it claimed was to give them the experience to pass the assessment processes the following year.
GP trainer’s view: ‘We are already feeling the fall in training applications’

I am a trainer and I like to train and teach. I am currently training a would-be GP, but I am worried there won’t be another one in the next allocation.
There has definitely been a fall in applications locally; we are feeling it already as GP practices. Trainees used to apply to general practice for a variety of reasons, such as flexible working hours and job stability.
But in the past five years, negative media coverage and the Government’s constant demands to do more with less have hit morale. This has put off young doctors, which is why we’re seeing a fall in applications for GP training in Walsall and across the Black Country.
In the long-term, if you have a look at the Five-Year Forward View, NHS England wants to move everything from secondary care to primary care. Who is going to do that work if the workforce is not there?
There is a mismatch between what they say and what the reality is.
It is already very difficult to find GPs for salaried posts, even with incentives. When I qualified in 2005, I had to go out and look for work.
I have been a partner for years and I have never before had companies approach me with offers of locum work. These days, my inbox is full with such requests.
Dr Uzma Ahmad is a GP trainer in Walsall, and a member of the GPC education and training subcommittee.
Efforts intensify
Dr Krishna Kasaraneni, chair of the GPC education and training subcommittee, says efforts to work together to boost GP numbers are taking place on a national scale now because the training crisis has the potential to ‘impede patient care’.
He adds: ‘We are working with the NHS England and HEE to find solutions to the issues, but we do believe that politicians of all parties need to provide additional support to enable more GPs to join the NHS workforce.’
There is no doubt that efforts to improve the recruitment of trainees have been stepped up.
NHS England released a 10-point strategy in January aimed at improving recruitment and retention of GPs, with ‘golden handshakes’ for graduates entering the profession, a marketing campaign aimed at young doctors and an additional ‘flexible’ year for GPs to train in a special interest.
This came a month after HEE had released its own workforce strategy, which set out plans to increase the number of GPs available for employment by 15% by 2020, work with the RCGP to attract more medical graduates to become GPs and commission a new GP workforce report on the numbers needed to provide NHS England’s new models of care.
The RCGP has already released a YouTube video telling medical students it is ‘the best time in a generation to become a GP’.
‘A lot more work for little reward’
However, as Dr Morton puts it, the reason behind the poor level of interest among graduates is ‘the impressions they have of primary care’.
A trainee himself, Mr Koneru would agree with this sentiment.
Having seen the effect the job had on his parents – who are both GPs – he has been put off the career for good.
He says: ‘It seems a lot more work for not much proportional reward.’
Mr Koneru says his fellow medical students keep up to date with what is going on in the profession and it is ‘absolutely the case’ that they have been put off general practice.
If NHS England and HEE are serious about increasing the numbers of GPs, they must take steps to ensure potential recruits are seeing a profession in a much healthier state.
GP training timetable
• 1 November 2014
Advert for applications for August 2015 entrance appears
• 4 December 2014
Closing date for first round of applications
• 3 January – 13 February 2015
Assessment of candidates
• 12 March 2015
Advert for second round of recruitment appears for positions not filled in the first round
• 26 March 2015
Successful first-round applicants informed
• 9 April 2015
Closing date for second round of applications
• 27 April – 15 May 2015
Assessment of candidates for second round of recruitment
• 29 May 2015
End of second round
• July 2015
Possible third round of recruitment
• August 2015
GP trainees from first two rounds of recruitment begin training