Missing millions: the broken promises on GP premises


empty waiting room 3×2
In the 2014 Autumn Statement, then Conservative chancellor George Osborne pledged a £1bn investment in primary care premises and technology over the next four years, saying this would underpin a ‘permanent improvement in GP services’.
It was a rare piece of good news for GPs. NHS England chief executive Simon Stevens said kick-starting an upgrade of primary care infrastructure was ‘mission critical’ and promised to get funding quickly to ‘shovel-ready’ projects, with longer-term projects prioritised in future years.
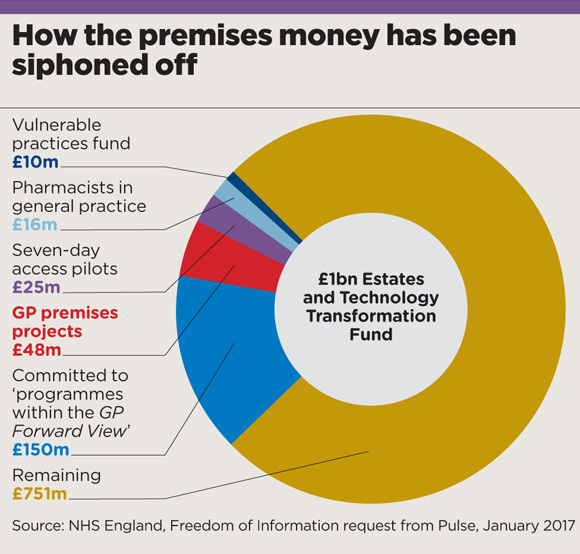
But halfway through programme the story is disappointing. Pulse has learned only 5% – £48m – of the £1bn ‘Estates and Technology Transformation Fund’ has been spent on premises.
Only a quarter of practices that have applied for funding have been approved, with many of those given much less funding than requested and sent back to the drawing board to make their projects deliver the same outcomes for less money.
Even worse, around £201m has been siphoned off to support other political projects and practices have been left to struggle on with growing lists and deteriorating buildings.
The figures obtained by Pulse under the Freedom of Information Act offer the first scrutiny of the fund, as NHS England has failed to publish its promised six- monthly reports on the scheme.
And Dr Peter Holden, deputy chair of the GPC finance and premises committee, says they show the fund has proved to be a Treasury ‘trick’.
‘They announce the money, and set an impossibly short application deadline so they don’t end up spending it because practices didn’t meet the deadline.’
Dr Holden should know – his practice applied to the fund. ‘We wanted to add consulting space. We’re hot desking as it is – I had to go home at lunchtime today to do paperwork because my room is needed by someone else. So we applied a few months ago, and got nothing.’
Promising start
When the fund was announced, GPC chair Dr Chaand Nagpaul said the announcement could help ‘begin to tackle the problems facing GP premises’ – but added ‘if delivered properly and in co-operation with GPs’.
And it started well. That March, more than 1,000 practices were pledged a share of £190m in principle, with those owning their own surgeries awarded a maximum of 66% of funding to complete the proposed development. But by November, there were clear signs that Dr Nagpaul’s caution was justified.
pulse premises money pie chart march 2017 580x554px
NHS England had rescinded millions in premises commitments, including from practices that had approval to start work. It also changed the terms of the funding, telling practices to redraw plans to match their CCG’s estates strategy, including buzzwords such as moving care out of hospitals and seven-day GP access.
Since then, the fund has gone through numerous rebrandings and name changes, and has been raided for other one-off projects, including £25m siphoned off for the second wave of the GP Access Fund, designed to increase weekend and evening routine appointments. A further £10m has gone to a fund for vulnerable practices – a noble cause, but one facing similar issues, with only £6m spent after 18 months.
And although it was also earmarked for improving practices’ IT infrastructure, NHS England was not able to give a figure on what it has spent, telling Pulse it had prioritised estates projects in the first year.
The demand is there. The scheme has been hugely oversubscribed, with NHS England funding just a quarter of the 2,000 submissions in the first year. In the second year, only 40% of the 2,000 bids put in by CCGs have been approved and even they are subject to due diligence, with no guarantee of funding as yet.
And there’s no doubt many GP premises are in dire need of improvement. In a 2015 survey of 527 practices by Cogora, the publisher of Pulse, one in 10 said they have hazards that could affect the health of patients and staff, while more than half lack the space to take on new staff.
A recent stipulation that CCGs must approve the plans has proved problematic as it can conflict with other priorities. In Leeds, commissioners say one in seven practices is unfit for purpose. Yet NHS North Leeds and NHS West Leeds CCGs have banned practices from applying where improvements might increase monthly rent reimbursements to GP premises, and therefore the CCGs’ costs.
Some practices receive no explanation of why they miss out on funding, including Dr Holden’s. Kathryn Hulme, practice manager of Mayfield Surgery, Stoke-on-Trent, says the practice is considering self-funding after its bid was rejected last year.
She says: ‘We have 11,800 patients with seven clinical rooms and 14 clinicians. Our bid has not been deferred, just not agreed as it did not fit NHSE criteria.’
Such uncertainty is jeopardising the future of general practice in some areas.
Dr Mike Hardman, a GP in Bridlington, East Yorkshire, and executive chair of local federation BridInc tells Pulse a new health centre is planned as a ‘world leading facility’ housing several of the town’s practices, after all were forced to close their lists due to unsustainable pressure. But though they received ‘initial approval’ for the £10.8m project, they are battling the ‘shifting sands’ of the funding rules, after NHS England revised the criteria.
Meanwhile, Kent LMC vice-chair Dr Gaurav Gupta says NHS England is using the situation to ‘twist their arms’. He was warned that funding to improve his Faversham practice premises could be pulled unless he signs a lease with NHS Property Services – against BMA advice.
This could expose Dr Gupta to increases in service charges that have been described as ‘crucifying’ by LMC leaders, and are currently under dispute.
As Dr Gupta puts it: ‘Our project is worth less than half a million but you’d think they were building the Gherkin.’
Pulse approached NHS England for comment but none was provided.
Rhetoric vs reality
Feb 2014
NHS England freezes all premises investment as part of a review of priorities for infrastructure funding.
December 2014
Chancellor George Osborne announces £1bn Primary Care Infrastructure Fund over four years to ‘deliver a permanent improvement in GP services’. NHS England chief executive Simon Stevens adds that ‘shovel-ready’ premises projects are to be prioritised in 2015/16.
March 2015
Over 1,000 practices provisionally awarded share of £190m in year one.
June 2015
Jeremy Hunt’s ‘new deal’ promises £10m for vulnerable practices and £15m to pilot pharmacists in general practice, but it transpires this is recycled money from the premises fund. He also says: ‘Over the next three years we will allocate the rest of this fund to further schemes so… cities and towns will see visible improvement in primary care facilities’.
July 2015
A further £25m is raided from the fund’s first year to support wave two pilots of extended evening and weekend GP access.
October-November 2015
NHS England rescinds millions in provisionally committed funding for premises improvements. It also rebrands the scheme as the Primary Care Transformation Fund and says bids must be signed off by CCGs, prioritising those that improve seven-day access.
April 2016
The GP Forward View says NHS England will change premises rules to allow it to contribute 100% of the premises costs for the next round of projects. It also pledges £50m a year from the premises fund to support other projects in the GPFV.
April 2016
The House of Commons Health Committee brands ‘siphoning off’ of funds from the newly named Estates and Technology Transformation Fund as ‘simply unacceptable’.
December 2016
NHS England says some 1,000 schemes – including premises and IT upgrades – have been provisionally approved.
March 2017
Pulse reports only £48m of the fund has so far been spent on premises.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens










