Revalidation – why it is time for a rethink


hammer v2 on yellow
It’s that time you dread. The moment you realise it’s just weeks until your final appraisal before revalidation.
The rush is on to complete enough CPD credits, get 360-degree feedback, amass reports on clinical audits or significant events, and include enough reflection on all of this to ensure your appraiser can tick all the relevant boxes.
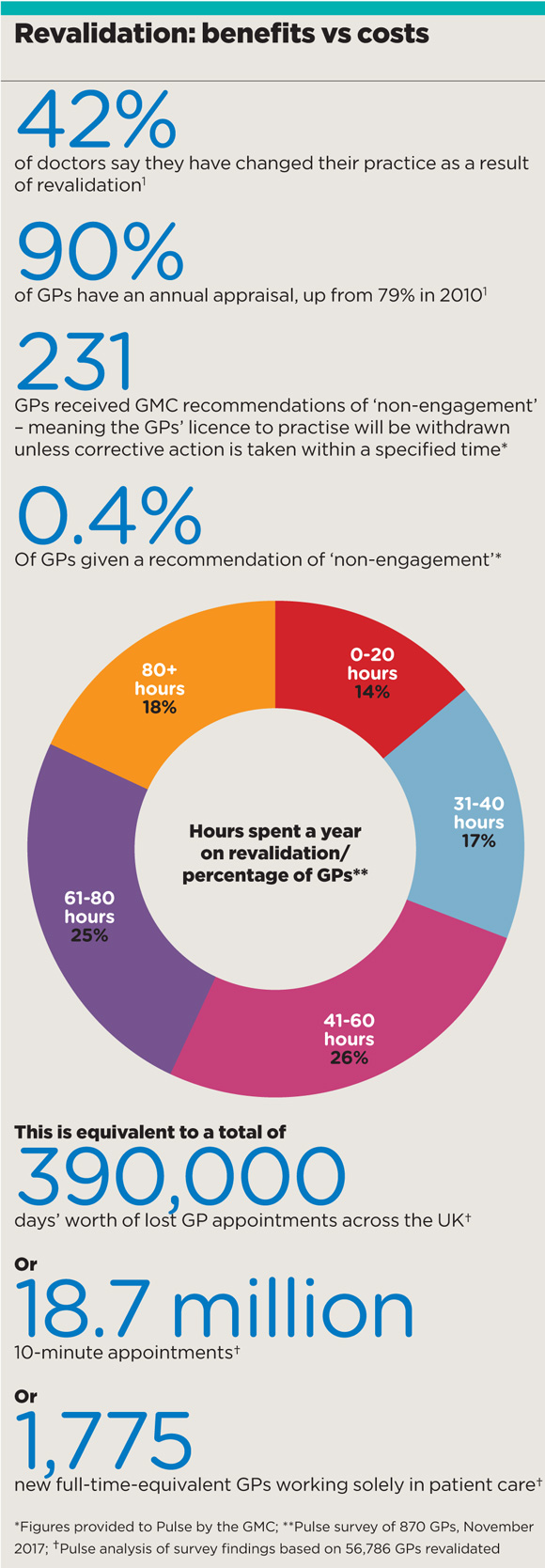
New figures from Pulse reveal the average GP spends around 55 hours a year preparing for their next appraisal. This is equivalent to a total of 390,000 days’ worth of appointments lost to patients at a time when many are waiting at least two weeks.
revalidation benefits vs costs 580x1668px
Put another way, this is the equivalent of the workload of 1,775 full-time GPs working eight sessions a week. This figure should be enough to give even health secretary Jeremy Hunt pause for thought.
And there is little evidence that all this activity has had any significant benefit. Just 231 of the 56,000 GPs revalidated provoked concerns serious enough for the regulator to threaten to withdraw a licence to practise.
A GMC-commissioned study of more than 26,000 doctors found that only 42% agree that appraisal is an effective way to improve clinical practice, with – incredibly – nearly 60% saying they have made no changes to their clinical practice, professional behaviour or learning activities as a result.
It was not meant to be this way. First proposed almost two decades ago, and then accelerated after the conviction in 2000 of GP serial killer Dr Harold Shipman, revalidation was meant to be a way to ‘restore confidence’ and drive up standards in the medical profession.
When it was implemented in 2012, it was touted as ‘the most significant reform of medical regulation for over 150 years’, with then GMC chair Sir Peter Rubin saying he was confident it would make a ‘significant contribution to the quality of care that patients receive’.
The Department of Health’s cost analysis at the time made the bold claim that revalidation would prevent 10% of the avoidable deaths and severe or moderate harm caused by doctors, and it would reduce litigation costs by 3%. It even projected that, ‘from 2017 onwards, a net benefit of around £50-£100m per year is expected to result, as revalidation beds in and the full benefits are realised’.
But when asked by Pulse recently, the department could provide no evidence these benefits had been realised, saying instead it was pleased revalidation had boosted the rates of annual appraisal for GPs by from 79% in 2010 to well over 90%.
A DH spokesperson said: ‘As highlighted in the Taking Revalidation Forward review in January, the process has delivered significant benefits through its appraisal system and strengthened clinical governance procedures.’
‘This is your opportunity – at a time when you’re nose to the grindstone – to stop and think and reflect and you should grasp it with both hands’
Dr Suzi Caesar, RCGP medical director for revalidation
That report, an independent audit of revalidation commissioned by the GMC last year, was carried out by the chair of Health Education England and the GMC’s Revalidation Advisory Board Sir Keith Pearson. It recommended several small changes to clarify the requirements doctors need to meet and to address the difficulties with getting meaningful colleague and patient feedback.
But the audit largely proclaimed revalidation a success. Sir Keith said in the report that revalidation was never intended to ‘catch another Shipman’. However, he added: ‘The array of governance changes put in place since Shipman, including those established as part of revalidation, makes it much more likely that his behaviour would have been detected earlier’. But the examples he listed – such as changes to death certification and closer monitoring of mortality rates – do not form part of revalidation and could have been implemented without it.
The RCGP – a supporter of revalidation from the start, and instrumental in its rollout – is also largely positive about the current regime. The college’s medical director for revalidation and member of the GMC’s revalidation advisory board Dr Susi Caesar says that, in the first few years of revalidation the pendulum inevitably swung towards too much box ticking, but adds: ‘Since Sir Keith did these interviews [in 2016] the pendulum has already swung back a lot.’
She adds: ‘The RCGP theme for the past two years has been increasing the value and reducing the burden.’ This includes an online mythbusters guide, which claims the final stage of getting together the supporting information for appraisal should ‘take no more than half a day’.
‘For every one rotten apple you’re probably driving 20 people out of the profession’
Dr Alan Woodall, founder of GP Survival pressure group
In 2016, the RCGP made changes to the system of CPD credits in an attempt to reduce the burden of documentation and simplify the process. It stopped GPs from claiming double points for demonstrating ‘impact’, but GPs said this simply meant they had to take more CPD modules.
Dr Caesar remains optimistic: ‘I say to GPs, this is your opportunity – at a time when you’re nose to the grindstone – to stop and think and reflect and you should grasp it with both hands.’
But the GPs say collecting evidence for appraisals is an ‘overwhelming’ task and is exacerbating the workforce crisis.
Powys GP and founder of the pressure group GP Survival Dr Alan Woodall says: ‘There has got to be a better way of monitoring and gathering evidence of unusual behaviour. For every one rotten apple you’re probably driving 20 people out of the profession.
‘For every hour of learning you can add another hour of recording and collating information. I spent three hours the other night on information governance and child protection, none of which required any real learning.’
Derbyshire GP and former BMA GP Committee negotiator Dr Peter Holden says: ‘It is about trust. No one else has to justify every step they take; nowhere else would stand for this degree of scrutiny.’
The BMA is demanding a rethink of revalidation. GPC deputy chair Dr Mark Sanford-Wood says although the union is supportive of it in principle, ‘considerable improvements’ need to be made.
He says the BMA’s figures on the time GPs spend on revalidation are lower than Pulse’s, but adds: ‘The time originally set aside was two sessions a year, one for preparation and one for the appraisal. But we know anecdotally that GPs spend considerably more than that putting together appraisal and evidence, probably in the region of four or five sessions a year – a significant chunk of time taken away from patient contact.’
He adds: ‘We need a national discussion about the evidence that’s required versus the delivery of patient care, particularly at a time when we just don’t have enough GPs to do that job.’
‘No one else has to justify every step they take; nowhere else would stand for this degree of scrutiny’
Dr Peter Holden, former GPC negotiator
But the GMC remains bullish: ‘Revalidation has helped strengthen the way we regulate doctors and embed a consistent approach to appraisal. Indeed, appraisal rates have risen steeply in all four countries of the UK since its introduction.
‘Doctors have said patient feedback is particularly valuable for identifying areas for improvement. Revalidation in turn plays a vital role in assuring patients their doctors are keeping up to date and have regular checks, maintaining confidence in the profession. But this is still just the beginning for revalidation and we don’t pretend the system is perfect.’
And the DH says: ‘It is vital doctors are able to reflect on and improve quality of care so patients can build a high level of trust and confidence in their doctors.
‘We continue to work with the GMC and other organisations to ensure the recommendations in the report are acted on effectively and provide maximum benefit to patients and doctors.’
But as West Sussex GP Dr Richard Cook points out: ‘Where is the proven benefit, where are the outcome data? It is using a sledgehammer to crack a nut. There has to be a better way.’
Indeed, it is disturbing that the regulator of a profession exhorted to follow the evidence base has no way of proving its methods offer any benefits at all to patients.
What is the alternative to revalidation?
While many countries around the world have medical standards similar to or even based on GMC core values, they do not have a national regulator overseeing the process.
US
Medical licences are issued at state level. The majority of licensing boards ask for doctors’ participation in CPD as part of the licence renewal process. The number of CPD credits required varies, with 50 per year at the top end of the scale.
Australia
For general registration with the Medical Board of Australia, doctors must complete a minimum of 50 hours of CPD a year. As specialists, GPs are required to meet standards set by the RACGP, which include undertaking two activities such as clinical audit in every three-year cycle.
Canada
Provincial colleges are responsible for regulating doctors. As part of annual licence renewal, doctors are ‘required to attest they are compliant’ with ongoing education. For GPs to maintain certification with the College of Family Physicians of Canada they must input at least 250 credits every five years into a computer program run by the college.
Germany
In Germany it’s all about self-regulation. A full licence to practise medicine is valid across the country for an unlimited period, with no revalidation or reaccreditation. All doctors must register with one of the 17 chambers of doctors, which set standards for specialist training and requirements for CPD, and enforce codes of conduct.
South Africa
The Health Professionals Council of South Africa is the medical regulator and made up of professional boards responsible for developing specific standards and policies. There is no regulation for revalidation but there is a requirement for ongoing CPD. Performance assessments are currently being considered for high-risk doctors.









