GMC: A more ‘compassionate’ regulator?


GMC 3×2
The GMC is trying to give itself a makeover, in the hope of becoming more ‘compassionate’ and ‘sensitive’.
Pulse has learned that the regulator has appointed an independent expert to ‘pinpoint’ ways in which it can ensure that its fitness-to-practise (FTP) processes offer greater support to vulnerable doctors.
Professor Louis Appleby – professor of psychiatry at the University of Manchester and chair of England’s National Suicide Prevention Strategy Advisory Group – has been recruited by the GMC to look at ‘every stage’ of the FTP investigation process and assess how it could be more caring towards vulnerable doctors.
And the GMC’s chief executive, Niall Dickson, tells Pulse in an exclusive interview that he recognises the regulator has an ‘absolute moral obligation’ to protect doctors as well as patients, conceding that it is time for its FTP procedures to be more ‘sensitive’.
GP leaders have welcomed Professor Appleby’s appointment as a ‘step forward’, saying it reflects a change of approach from the regulator.
The appointment follows what has been an uncomfortable 12 months for the regulator, with a handful of studies suggesting the FTP procedures must be improved.
A GMC-commissioned review at the end of 2014 found 28 doctors had died while under investigation and concluded that doctors could become ‘marginalised’ during the FTP process and receive little support or compassion from the regulator.
Another review published last year said 13 doctors died while the GMC ‘failed to act’ after concerns were first raised about the high numbers of doctors dying by suicide while under investigation.
We want to be as compassionate as we possibly can be with all doctors
GMC chief executive Niall Dickson
It said the GMC should have ‘immediately ceased’ its fitness-to-practise cases and ‘urgently reformed’ processes after concerns were first raised in 2012.
Another study last year went as far to say that complaints against doctors ‘may do more overall harm than good in terms of patient care’, as the majority of doctors who are reported to the GMC are found to have no significant case to answer.
Toxic impact
The shocking study of 8,000 doctors by researchers at Imperial College London highlighted the toxic impact the GMC’s complaints procedure has on the mental health of doctors – with one-sixth saying they had suffered severe or moderate depression following a complaint, and many others reporting anxiety and even suicidal ideation.
Perhaps, though, the most worrying finding from the study was the adverse effect on patient care. Some doctors admitted they changed the way they practise following a complaint, with one in four saying they had suggested invasive procedures against their professional judgment.
Since then, the GMC has formulated an action plan to implement recommendations from its own review, and says it has already changed the tone of its correspondence with doctors who are under investigation.
But it intends to go further. Mr Dickson tells Pulse: ‘We’ve already started mapping our process very carefully and look at each individual stage that we go through. And what we want Professor Appleby to do is to review that process and advise us on further things that we can do within our current legal powers.’
He says that while the GMC’s core duty to protect patients will remain, there is an important role to be played in providing support to doctors who are under investigation.
‘We absolutely want to be as compassionate as we possibly can be with all doctors, not just those who have mental health problems, but all doctors who are in our FTP procedures.’
GP leaders have welcomed the move. Former RCGP chair Professor Clare Gerada, who is medical director of the Practitioner Health Programme – a support service for sick doctors – told Pulse that the announcement of Professor Appleby’s review ‘shows a shift in the last two or three years at the GMC’.
She added: ‘I think it is good news for everybody – because the pendulum of regulation that is anti-doctor is beginning to swing back to a more healthy place, where doctors can be mentally ill – yet trying their best in very difficult times.’
Professor Appleby has already tweeted that he has heard from ‘several doctors’ since Pulse revealed his appointment and that feeling ‘guilty until proven innocent’ was a common theme.
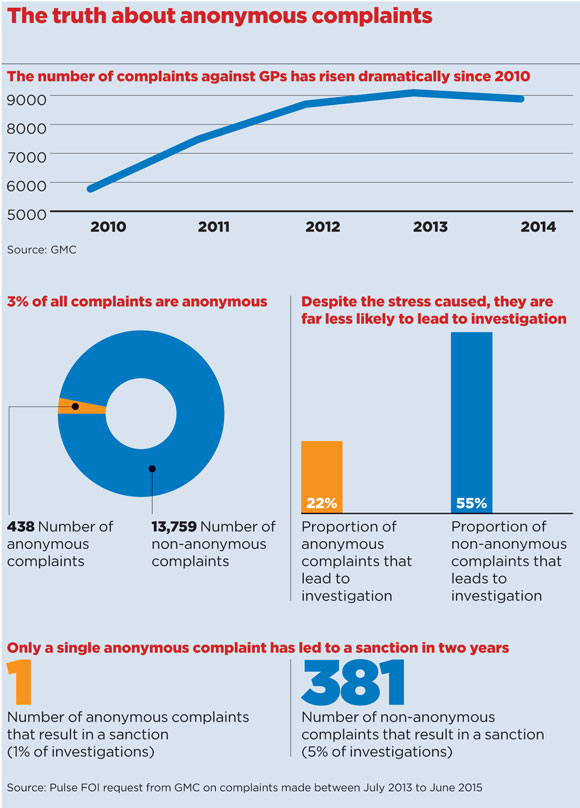
The number of doctors undergoing FTP investigation has risen significantly, by 54% since 2010. But more than half of cases result in no action being taken against the doctor – leading to further calls for the system to be reformed.
New GMC figures show the number of complaints against doctors remains high, with 8,884 in 2014 and 9,093 the previous year.
But the proportion of investigations that lead to no action being taken is increasing, reaching 48% in 2014, compared with 44% in 2013.(3)
Empty complaints
Meanwhile, figures obtained by Pulse from the GMC, reveal that only one anonymous complaint against a doctor has led to a sanction over the past two years.
The figures, which are based on complaints made from 2013 to 2015, show that of 438 anonymous complaints, 97 led to an investigation being launched by the GMC – but only one of these actually led to a sanction being imposed. GP leaders say this raises serious concerns about the weight given to anonymous complaints.
BMA chair Dr Mark Porter told Pulse he was concerned about the implications of the figures.
He said: ‘Doctors strive to deliver the best possible care to patients and it is right that we have a robust system that ensures any problems that do occur are addressed. However, it is clear from these figures that, in the vast majority of cases, doctors are exonerated when complaints are made.
Dr Porter added: ‘Complaints procedures need to be efficient and fair. At present, doctors who are the subject of a GMC investigation can be left in limbo for months, or even years, before an outcome is reached. The stress that this causes to those affected can have life-changing effects.
‘While doctors always want to learn from clinical mistakes, it’s also important that the GMC learns from the way its systems operate. It is clear from these figures that anonymous complaints seem to be given undue weight in the complaints process.’
But Mr Dickson points out that the GMC is often legally obliged to act on every single complaint, even if in many cases no action is subsequently taken by the regulator.
He explains: ‘From the doctor’s point of view, that’s awful, because we’ve subjected [them] to all this anxiety over a period of time. From our point of view, we do it because the law says we have to do it, so what we have to do is try to find every way we can to reduce that amount of time.’
Mr Dickson adds that Professor Appleby will be tasked with recommending any legal changes that the GMC can lobby the Government to bring forward to ‘make the system better’.
The medical profession will be hoping he does a thorough job.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens












