Screening the masses: GPs set for contractual incentives to measure diabetes risk

GPs are at the forefront of a major drive to improve the nation’s unhealthy lifestyles.
NHS England chief executive Simon Stevens has fired the starting pistol on a national project to make England ‘the best country on the planet’ at preventing type 2 diabetes.
Pulse has learned that GPs could face contractual incentives to encourage them to find the 10 million people in England at high risk of developing diabetes.
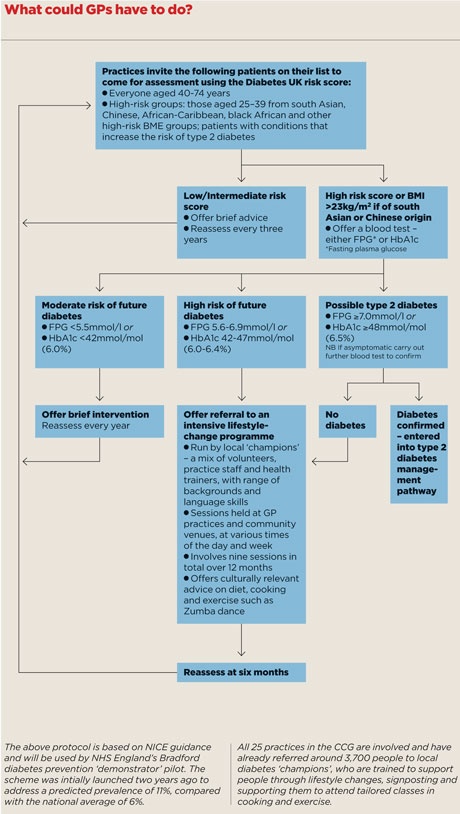
Managers want GPs to go through their patient lists and refer those at high risk for interventions, such as Zumba dance and cookery classes.
The project will be piloted in seven areas this year and then launched nationally from next April.
But the GPC has warned practices are already ‘oversaturated’ and that improving access to healthier food and exercise should also be a priority.
The Diabetes Prevention Programme is the most ambitious project since the NHS Health Checks scheme was launched five years ago by then Prime Minister Gordon Brown.
But the health checks scheme has not been a roaring success, being implemented in a piecemeal fashion, with studies suggesting it failed to increase diagnoses of vascular disease beyond the usual opportunistic testing in primary care.
30% cut in incidence
Despite this, NHS chiefs are confident the new scheme will cut the incidence of diabetes by at least 30% and tackle one of the greatest dangers to the future sustainability of the health service.
It will start this year with seven ‘demonstrator’ sites across the country involving hundreds of practices evaluating various models of screening and lifestyle prevention in around 10,000 high-risk patients.
At five of the seven sites – Birmingham South Central, Bradford, Medway, Salford and Southwark – GPs are being incentivised to take the NICE-recommended approach, systematically creating a register of people at risk of diabetes, carrying out regular reviews of people on the register and giving them tailored management plans, including referral to intensive lifestyle-change programmes. Salford’s programme also includes a telephone-based support service.
Two areas will run a modified NHS Health Checks scheme, with GP practices in Durham using the Diabetes UK score for the initial assessment, to capture more people at risk of diabetes, and GP practices in Birmingham South Central carrying out an HbA1c blood test on everyone aged 40-74 invited in for the check, not just those found to be at risk by the initial assessment.
Both Birmingham and Herefordshire will also broaden attempts to identify people and add them to GP practice risk registers for follow-up, including screening of people visiting hospitals for pre-operative assessments or routine procedures.
Enthusiasm
The project fulfils one of the major aims of NHS England’s Five Year Forward View – which promised a ‘radical upgrade’ in prevention and public health – and GPs with an interest in diabetes have greeted it with enthusiasm.
Professor David Haslam, chair of the National Obesity Forum and a GP in Bedfordshire specialising in obesity and diabetes, says: ‘It certainly seems [NHS England] have twigged that – as we have been telling them all along – if diabetes doesn’t get sorted out, that’s the end of the NHS.’
Similarly, Professor Kamlesh Khunti, professor of primary care at the University of Leicester, who led on the NICE diabetes prevention guidelines, says: ‘We have been calling for this for a while. It’s nice to see it has finally been made a priority.’
But the GPC is unimpressed. Chair Dr Chaand Nagpaul says: ‘General practice is already oversaturated and there are many factors that create obesity. Simply giving practices incentives isn’t going to solve the UK’s rising rates of obesity.’
He points out that there is little value in diagnosing diabetes if there is no easy access to affordable exercise programmes or enough trained counsellors, adding that the ‘mantra that everything has to be done through GPs’ has to stop.
He says: ‘It does not necessarily need a GP’s time. We should look at hospitals, schools, pharmacists and workplaces – we should not be looking towards funnelling every element of health promotion through the GP practice.’
The GPC has also been quick to point out that the NICE guidelines on preventing diabetes have not been taken up in primary care for these very reasons since their publication in 2012. A Pulse investigation 2013 found GPs in 42% of areas across England did not have access to intensive lifestyle change programmes for patients at risk of diabetes.
In a report to MPs, Public Health England recently said it wanted to see incentives for GPs to refer overweight patients for weight-management schemes placed in the QOF.
But despite assurances that GPs will be able to refer patients to suitable programmes, some question the evidence behind the scheme.
Dr John Ashcroft, a GP in Derbyshire and GPSI in cardiovascular medicine, says diet and exercise are unlikely to be effective outside trials and that it is more probable that people will end up being given metformin.
He said: ‘The most cost-effective, and at a population level, probably the most effective, management is metformin.
‘People think that it is diet and exercise, but metformin is much cheaper and probably more applicable at a population level rather than intense exercise and weight-loss regimes applied to highly selected groups, such as those identified [in this programme].
‘Metformin is recommended by NICE, but again entails more unresourced work managing “pre-diabetes” for GPs.’
And that is the concern for many GPs, that – despite the scheme’s merits – it comes at a time of unprecedented workload and a recruitment crisis in the profession. The last thing many practices need is to take on a gargantuan public health drive, and they will hope that NHS England’s initiative does not end up being just that.
What is the evidence for type 2 diabetes prevention?

• The Diabetes Prevention Program Research Group in the US studied some 3,200 overweight men and women, with elevated fasting and post-load plasma glucose concentrations. Over 2.8 years of follow-up, an intensive lifestyle intervention reduced the incidence of type 2 diabetes by 58%, compared with placebo, at 4.8 versus 11.0 cases per 100 person-years.
NEJM 2002; 346: 393–403
• The Indian Diabetes Prevention Programme in more than 500 men and women found lifestyle modification cut three-year cumulative incidence of type 2 diabetes from 55% to 39% compared with control – a 29% relative risk reduction.
Diabetologia 2006; 49: 289–297
• China’s Da Qing Prevention Study of nearly 600 people with impaired glucose tolerance, showed diet and/or exercise interventions cut the cumulative incidence of type 2 diabetes over six years from 68% to between 41% and 46%, compared with controls – with relative risk reductions of 31%-46%.
Diabetes Care 1997; 20: 537–544
• A Finnish study in more than 500 middle-aged, overweight men and women with impaired glucose tolerance showed an intensive lifestyle intervention cut the incidence of type 2 diabetes by 58% over three years; 11% who received the intervention went on to develop diabetes, compared with 23% of the control group.
NEJM 2001; 344: 1343–1350
But practices may now have little choice in the matter. Pulse has learned that managers are now looking at contractual incentives to encourage practices to participate in the identification programme.
Dr Jonathan Valabhji, NHS England’s clinical director for diabetes and obesity, says the national strategy is likely to involve ‘levers’ such as the QOF and enhanced services. ‘We’re exploring those options – it’s an obvious place to look, computer systems can generate a register of those at high risk of diabetes.’
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.










