Are GPs suffering from ‘sepsis fatigue’?
c0345870 sepsis, sem science photo lib 3×2
After spending years in the shadows, sepsis has become a cause célèbre. Rising death rates have prompted national headlines and prompted an NHS-wide drive to ensure cases are not missed.
But GPs have been caught in the crosshairs. Of the many infections that present in primary care, only a fraction will progress to such serious complications. There is no laboratory test that can confirm or exclude sepsis; instead a raft of symptom scores have been embedded in GP IT systems leading to ‘alert fatigue’ and some GPs simply switching them off.
Even NHS England has admitted that recent NICE guidance on sepsis – which listed numerous warning signs that should prompt referral – has proved too complicated to implement.
Commissioning guidance released in September conceded that ‘some front line staff have found it difficult to translate this guidance into practice’. It goes on to say that: ‘The application of the recommendations in the NICE guideline NG51 is not mandatory and the use of clinical judgement is a critical component.’
Dr Green said: ‘The largest problem with it is the low threshold for sending an alert. The result is that these alerts are ignored. Should that “suspected UTI” patient go on to have sepsis, GPs may find themselves having to justify why they did not take action earlier. Inquests where people have ignored warnings rarely look at the contribution of alert-fatigue.’GPs faced with innumerable pop-ups based on the NICE guideline and urging them to ‘think sepsis’ agree. BMA GP Committee prescribing lead Dr Andrew Green says the electronic scores based on the NICE guidance and put into GP clinical systems represented ‘a lesson in how not to use IT’.

dr green, andrew charles milligan 3×2
Even enthusiasts agree. Chief executive of the Sepsis Trust Dr Ron Daniels admits the alerts were implemented ‘hastily’ and have backfired in some cases. He says: ‘We’re aware of anecdotal cases where GPs have found the systems very helpful in clinical decision making, but we’ve also heard of cases where GPs decided to turn off the alerts.’
The Government drive began two years ago with a string of measures designed to make GPs ‘think sepsis’ after a series of high-profile deaths. The 2015 sepsis action plan suggested GPs have limited ability ‘to distinguish between sepsis, severe sepsis and septic shock’ and urged doctors to use screening tools to help differentiate simple infection from something more serious.
GP leaders said at the time this criticism was unfair as sepsis was hard to spot and the profession was also under pressure to cut antibiotic prescribing. But in 2016, NICE piled in with its guideline urging GPs to treat signs of sepsis in the same way as chest pain and including large tables of symptoms and signs designed to show whether a patient is at high risk of severe illness or death from sepsis, and requires referral if present. These were then quickly translated into electronic alerts embedded into GP systems.
Warwickshire GP and RCGP Council member Dr John Cosgrove says the alerts can be helpful in listing what information GPs should record. However, some ambulance services – inundated with demand – are using the data received from GPs to downgrade the urgency of ‘blue light’ calls.
He adds: ‘We have been trained since we were medical students to detect sepsis and respond appropriately. This should be given more respect, not less, including a more sophisticated awareness that clinical judgement is not infallible and indeed that the symptoms and signs of sepsis overlap with other conditions.’
RCGP clinical champion for sepsis Dr Simon Stockley says there must be greater recognition of the importance of clinical judgement in assessing the risk of infection – mirroring the recent NHS England advice that he co-authored.
Dr Stockley says: ‘The numbers will not always give you the right answer, which is why the clinical systems tend to over trigger. You should always use your clinical judgement to weigh the risk.’
A recent survey of 800 GPs supported this viewpoint, finding the decision to refer a patient to hospital with possible sepsis to be a ‘complex diagnostic process’ and warned that making a decision based purely on vital signs disregards important clinical information.5
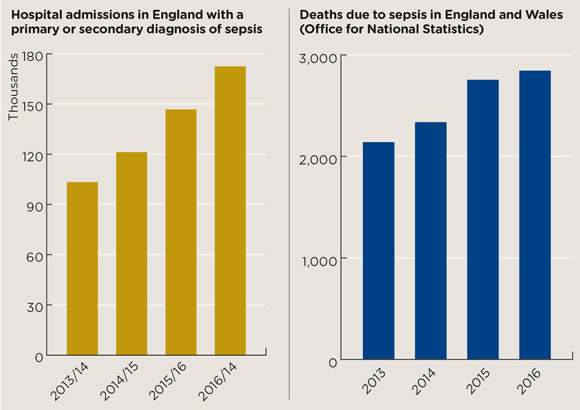
sepsis bar chart nov2017 580x410px
Sources: Hospital Episode Statistics (HES), NHS Digital, Office for National Statistics
NHS England’s latest advice indicates that it might be listening, but the sepsis bandwagon rolls on. Despite some negative feedback from GPs, the Government referred to the ‘successful delivery’ of the interventions last month, when it announced further measures to tackle sepsis.
The ‘second sepsis action plan’ focuses on nurses, care home staff and pharmacists, and includes more changes for GPs. Themes include prevention, improving identification, and ‘safety netting’ for cases where a patient with infection has been assessed not to have sepsis but is given information on signs to look out for. The plan also details yet more revisions to sepsis detection software, including the rollout of the ‘GRASP-Fever’ tool to help GPs manage children presenting with fever.
This will not replace the existing screening tools, although managers say they will work with GP software providers to ‘update their sepsis alert algorithms’.
‘GP software providers have been asked to include sepsis safety-netting resources that GPs can pass on to patients/carers, especially the parents of children with infections,’ details the NHS England plan.
Sepsis is also becoming a policy priority outside England. In September, a national awareness campaign was announced in Scotland, despite the Scottish Government stating just weeks earlier that such a campaign was unnecessary.
After a meeting with the Fiona Elizabeth Agnew Trust (a charity set up by the husband of a Scottish GP who died from sepsis in 2012), Scottish health secretary Shona Robison said a marketing and awareness campaign was the ‘sensible next step’. The details of the campaign have yet to emerge, but adverts are expected to reach more than a million people in Scotland, alongside work by Healthcare Improvement Scotland to raise awareness among doctors.
Dr Stockley concludes: ‘The guidance has made a good start, but there are things still left to do and challenges ahead, particularly in terms of being able to measure impact.
‘We’ve tackled many of the major killers with new medicines, or better organisation to apply the treatments we already know work, but we haven’t done this systematically with sepsis, partly because it is so difficult to detect and manage. But just because it’s difficult doesn’t mean we shouldn’t tackle it.’
Progress so far: the sepsis drive
Official NHS figures show admissions for sepsis have increased by more than 66% since 2013, and by more than 17% since the 2015 sepsis action plan was introduced (see below). Deaths are still rising, but the rate of increase has slowed. In 2015, there were 2,754 deaths – up 18% on the previous year, compared with a rise of just 3% in 2016.
The data on sepsis are inaccurate and unreliable Dr Ron Daniels
But these figures could just be due to greater recognition and better coding, and many cases may still be missed. Dr Ron Daniels says the Sepsis Trust estimates that 37,000 people die of sepsis each year in England, and 44,000 each year across the whole UK.
‘The reality is we don’t know,’ he says. ‘At the moment figures on sepsis are reliant on coded data, which can be inaccurate and unreliable… We know at least 20,000 patients died of sepsis on intensive care units alone last year, which makes a complete mockery of the ONS data.’
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Visit Pulse Reference for details on 140 symptoms, including easily searchable symptoms and categories, offering you a free platform to check symptoms and receive potential diagnoses during consultations.









